Informed Policy, Strong Systems


Vaccines save lives. Health system improvements do, too. Through research and implementation support, Abt helps governments ensure the delivery of high-quality, cost-efficient healthcare, rooted in the best evidence. We strengthen health policy, assess healthcare needs and insurance coverage gaps, and implement solutions to deliver care to those that need it most.
Informing Health Policy
Abt works to advance health policy around the world, with an emphasis on realizing value-based health systems that synchronize incentives to deliver high-quality, accessible care in a patient-centered environment.
In the United States, improving the nation’s health has been a key focus of ours since our founding in 1965. Clients have sought our expertise to expand access to quality care, support payment policy and service delivery reforms, determine policy and program effectiveness, and reduce health disparities.
Evaluating Innovations
Abt evaluated a federal grant designed to improve care in hospital intensive care units (ICUs) by enabling specialized physicians, intensivists, to have telepresence in multiple ICUs.
ICUs treat particularly critical patients, and research has shown that patients treated by intensivists have the best outcomes. The tele-ICU was designed to mitigate a national shortage of intensivists by allowing one specialist to cover several ICUs.
Our analysis indicated that the tele-ICU reduced spending by an average of $1,486 per episode of care among Medicare beneficiaries in the ICU, without increasing hospital readmissions or visits to institutional post-acute care facilities. Overall, we estimated that the tele-ICU saved Medicare $4.6 million over the first 14 months of operation, demonstrating the promise of tele-ICU systems.
Project Evaluating Health Care Innovation Awards for Hospital Setting Interventions
Funder Centers for Medicare and Medicaid Services (CMS)
Addressing Housing as a Social Determinant of Health for People with Disabilities
Medicaid provides critical assistance that enables people with limited incomes to access medical care and long-term services and support. The Medicaid Innovation Accelerator Program (IAP) provides targeted resources to state Medicaid programs to support their ongoing efforts to innovate towards payment and delivery system reform. As one component of our overall evaluation of the Medicaid IAP, Abt is assessing the development of partnerships between state Medicaid and housing agencies to foster additional community living opportunities for Medicaid enrollees with disabilities. Our rapid cycle evaluation documents the evolving IAP-enabled partnerships and how CMS’ real-time refinements to the program helps states address housing as a social determinant of health. Early results suggest the IAP successfully strengthened partnerships.
Project Evaluation of the Medicaid Innovation Accelerator Program
Funder Centers for Medicare and Medicaid Services (CMS)
Evaluating Incentives to Test New Payment Models of Care
The Centers for Medicare & Medicaid Services established a range of alternative payment models with the goal of transforming the traditional Medicare program from a volume-based model to one based on value. Accountable Care Organizations (ACOs) that participate in the Medicare Shared Savings Program represent an alternative payment model comprising voluntarily convened groups of physicians, hospitals, and other health care providers responsible for the cost and quality of care of the patients who visit them most frequently.
Financing and inadequate capital have been cited by rural providers as significant obstacles to ACO participation. To address this barrier, the ACO Investment Model (AIM) provides up-front financial support for care transformation to eligible ACOs. Abt studied whether AIM effectively increased and sustained provider participation in ACOs as well as whether the model had an effect on Medicare spending and quality of care.
We found that reductions in Medicare spending and utilization did not result in lower quality of health care, with most AIM ACO’s reporting they would not have participated in the Shared Savings Program without AIM funding.
Project Evaluation of the ACO Investment Model for the Center for Medicare & Medicaid Innovation (CMMI), CMS.
Funder Centers for Medicare and Medicaid Services (CMS)
Reforming Health Financing in Ethiopia
In Ethiopia, per capita health spending in 2016/17 was only $33 per year, with nearly one-third of that being out-of-pocket expenditures. This high share of out-of-pocket spending often made health care prohibitive for households, or proved financially catastrophic for those who did access health services. Health facilities had inadequate operational budgets, leading to a lack of diagnostic equipment, drug shortages, and facility infrastructure in need of repair. These problems contributed to the low quality, availability, and utilization of health services across the country.
To improve the quality and availability of services, Abt worked with the Ethiopian government to implement a number of health finance reforms. Between 2011 and 2019, Abt’s technical assistance helped 92 percent of health centers and 99.7 percent of hospitals retain revenue and then use the retained revenue to significantly improve the quality of services offered. The share of the internally generated revenue has on average reached over 30 percent of health facility budgets.
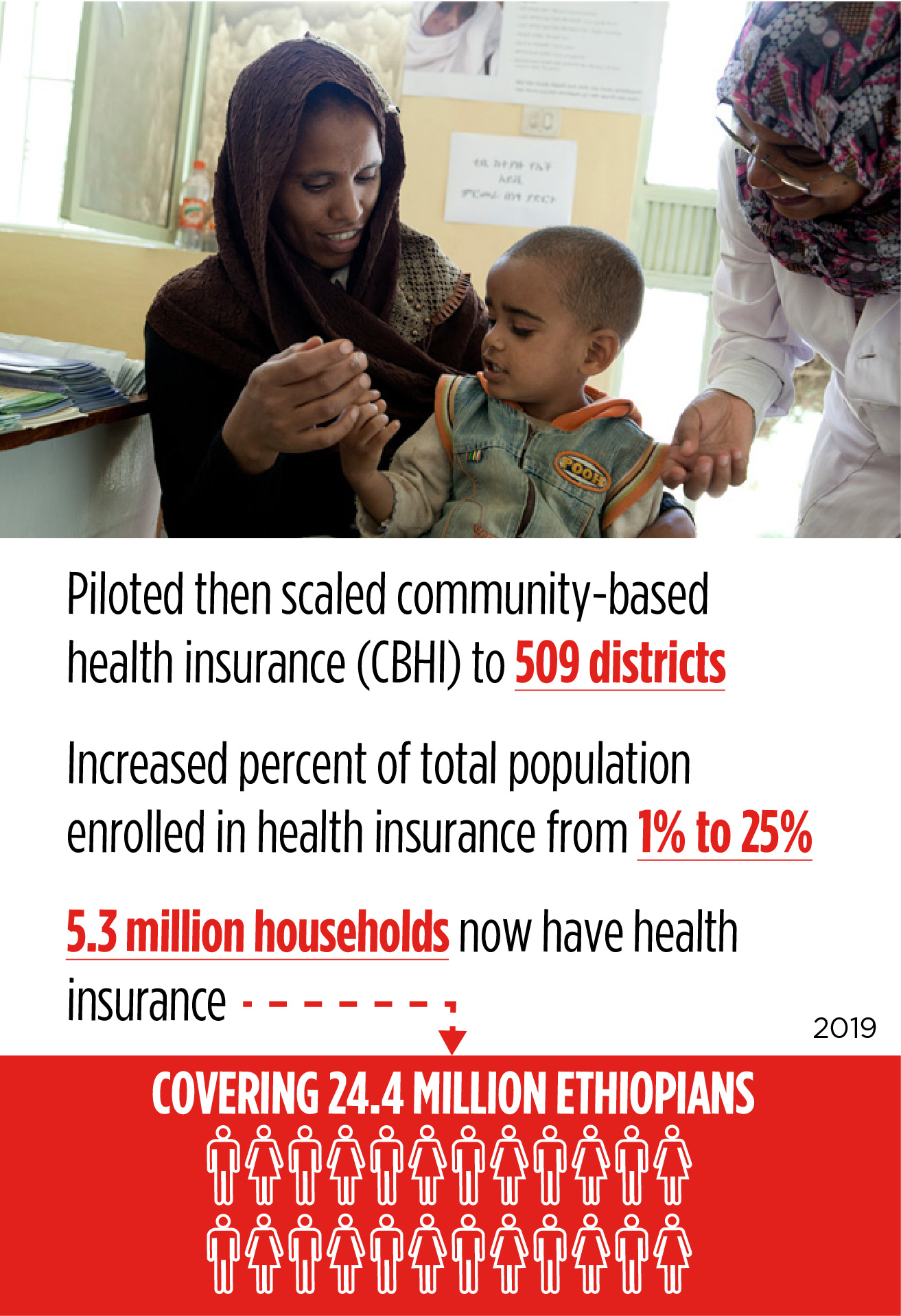
To improve financial protection for patients and the utilization of health services, Abt helped to significantly expand Ethiopians’ access to health insurance through community-based health insurance (CBHI). CBHI is a risk pooling mechanism through which members from the informal sector pool contributions into a collective fund that covers health care expenditures at health centers and hospitals. Abt helped pilot CBHI in 13 woredas (districts) from 2011-2013 and then evaluated to identify lessons to inform scale-up. The evaluation showed that CBHI members used health services almost twice as much as the national average and were 26 percent more likely to seek care when sick compared with non-members. Abt then helped scale CBHI to more than 500 woredas, to date providing health insurance to 24.4 million people.
Project USAID Health Financing Improvement Program; Transform: Primary Health Care; Health Sector Financing Reform (HSFR), Health Finance and Governance (HFG)
Funder U.S. Agency for International Development (USAID)
Strengthening Senegal’s Health System
Abt has led health system strengthening programs in Senegal for more than 20 years, building critical foundations for implementing sustainable health reforms and working with the Government of Senegal to develop its universal health coverage (UHC) strategy. Abt’s contributions include helping to develop the national UHC legislation, increasing private sector involvement in mutuelles (community-based health insurance programs—CBHI), improving participation in, and governance of, CBHI, and facilitating political and technical dialogue to help expand health-related financial risk protection for the population.

With Abt’s assistance, the government developed a strategic UHC plan and agency—Agence de la Couverture Maladie Universelle, established in 2015. Between 2011 and 2015, Abt’s technical assistance contributed to the creation of more than 100 CBHI schemes that are providing financial protection to more than 700,000 people. Since 2016, an additional 50,000 people have joined CBHI schemes as Abt continues to work with Senegal’s UHC Agency and local community-based organizations to expand access to insurance.
Project Health System Strengthening (HSS);Health System Strengthening Plus (HSS Plus)
Funder U.S. Agency for International Development (USAID)
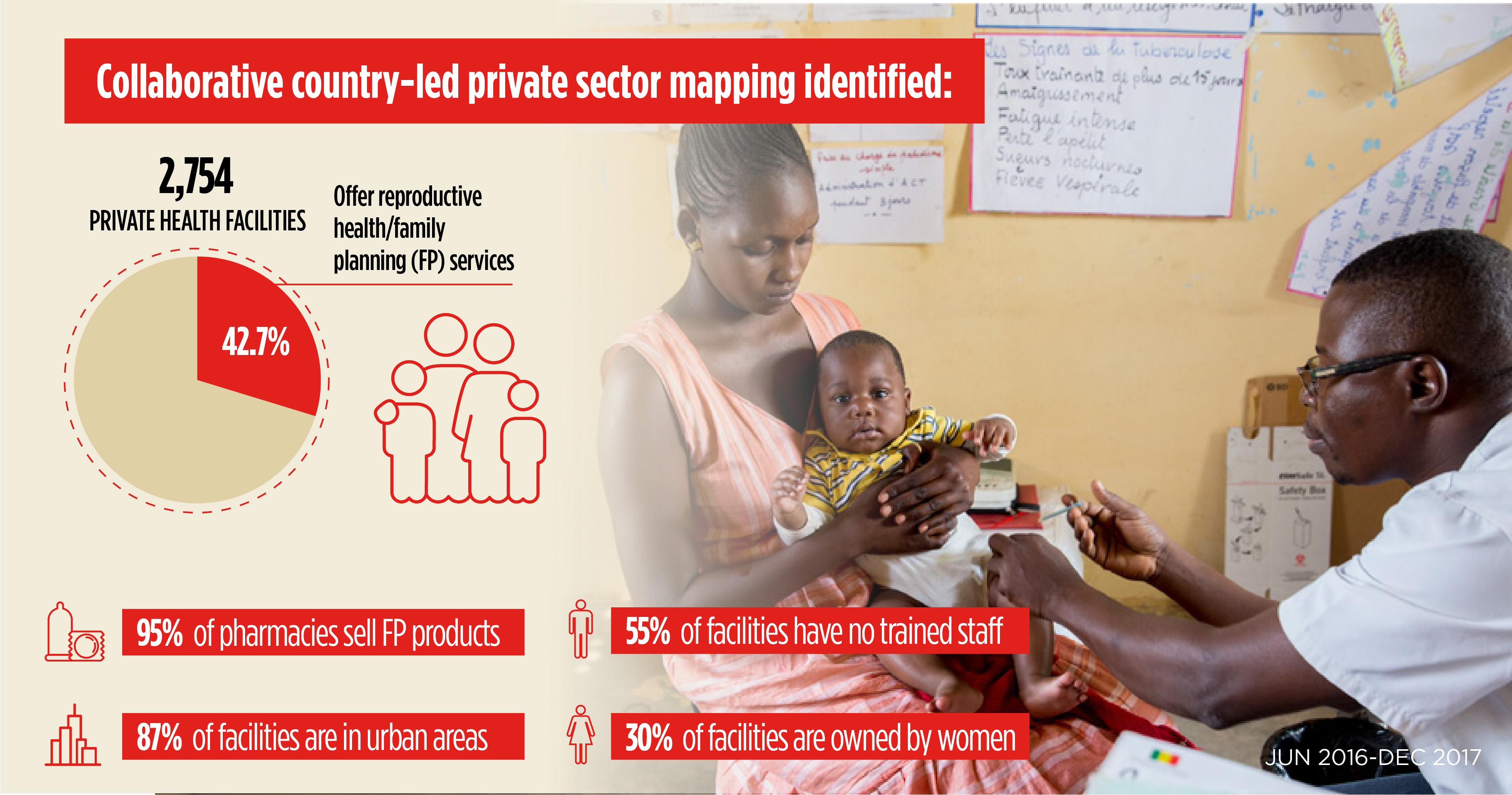
Improving Health Sector Understanding through a Collaborative, Country-Led Approach
Public and private stakeholders in Senegal need to better understand the scale and scope of the private health sector, including all private health practices and the full range of facilities offering services. Abt completed a new private sector mapping study—in partnership with the Ministry of Health and Social Action (MSAS) and USAID—to provide policy makers, health professionals, and stakeholders with a more accurate picture of the private health sector. Abt is using the mapping data to identify private facilities for a quality improvement pilot intervention, to advance the delivery of priority health services, including family planning (FP).
This mapping study was the result of a collaborative effort among multiple stakeholders, including the MSAS, the Alliance of Private Health Providers, and professional associations, all of which were involved in study implementation, data validation, and dissemination results. The Public-Private Partnerships Technical Committee of the MSAS provided oversight, with buy-in from the regional and district-level health authorities. This collaborative approach was instrumental in ensuring that the findings get used and integrated into future programs and policies.
Project Sustaining Health Outcomes through the Private Sector Plus (SHOPS Plus)
Funder U.S. Agency for International Development (USAID)
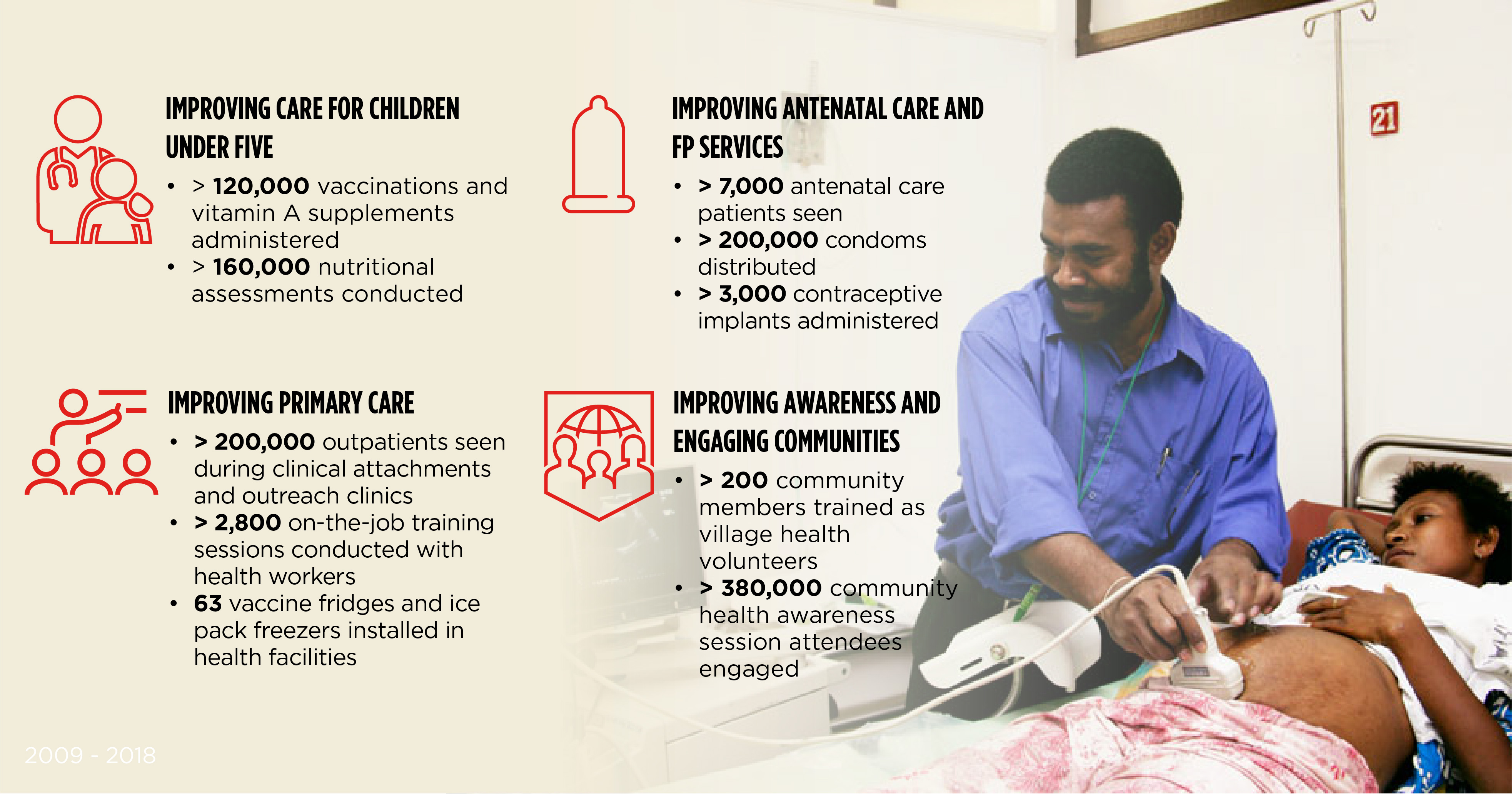
Improving Primary Health Care Services in the Western Province of Papua New Guinea
Papua New Guinea (PNG) faces significant health challenges, including some of the highest rates of maternal mortality, low vaccination rates, and increases in malaria, polio, and tuberculosis. Abt led two longstanding comprehensive programs to improve core primary health care components in the Western Province of PNG: the North Fly Health Services Development Program (2009 to 2018) and the Community Mine Continuation Agreement Middle and South Fly Health Program (2013 to 2018). The two programs (merged in 2016) resulted in significant improvements in health across the province.
Abt facilitated coordination among key institutional stakeholders, ensuring the fundamental building blocks of health care were available across all health facilities supported by the programs. This included a capable and available health workforce, and an adequate supply of drugs and equipment. Abt focused on improving child and maternal survival and reducing the burden of communicable disease.
Project North Fly & South Fly
Funder Ok Tedi Development Foundation
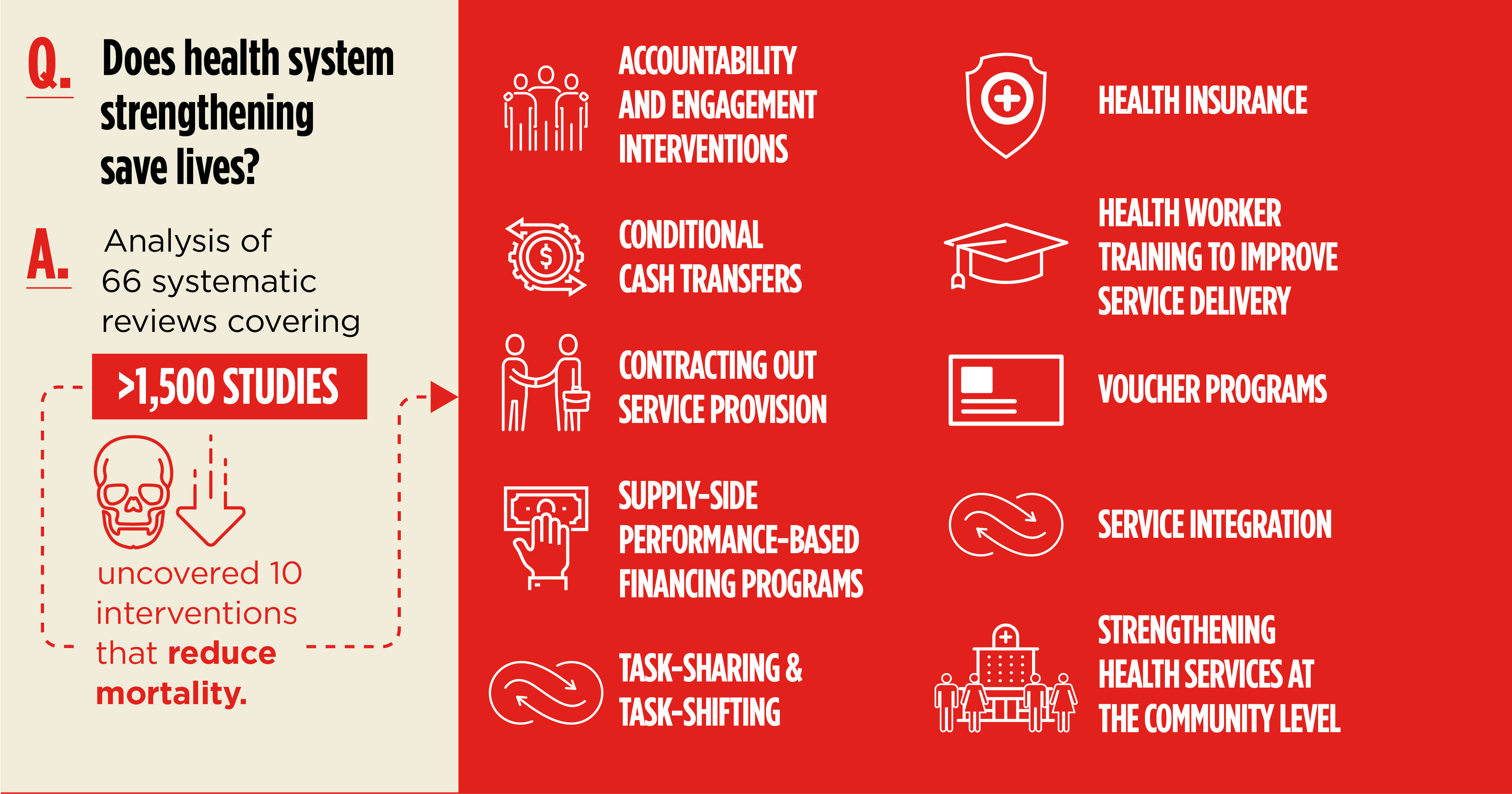
Illuminating Impact of Health Systems Strengthening on Health
A myriad of potential health systems strengthening interventions—from digital health support, to conditional cash transfers for the poor, to service integration at the clinics—represent competing options for decision makers looking to invest health funds in solutions with robust evidence of effectiveness. But the impacts of health systems strengthening initiatives on health status and related outcomes had not been comprehensively reviewed. To address this knowledge gap, Abt conducted a review of published systematic literature reviews that assessed the effects of health system interventions in low- and middle-income countries.
Abt researchers identified 66 systematic reviews that met the inclusion criteria for analysis; together, they covered more than 1,500 individual peer-reviewed studies. This review found evidence that health systems strengthening interventions produce substantial positive effects on health status and health system outcomes. Specifically, we identified 13 types of interventions associated with reductions in morbidity for a range of conditions, including diarrhea, malnutrition, low birth weight, and diabetes, including 10 associated with reductions in mortality. Health systems strengthening interventions are also associated with improvements in service utilization, financial protection for individuals and families, and provision of high quality services.
Project Health Financing and Governance (HFG)
Funder U.S. Agency for International Development (USAID)
Improving Quality of Health Services
Quality through Transparency and Quality Ratings
Transparency in provider performance is key to promoting high quality healthcare, especially for vulnerable populations such as older adults and people with disabilities and chronic conditions. In the United States, Abt and partners developed, tested, and implemented quality measures—including star ratings that combine multiple measures—for home health services, hospice care, and nursing homes.
Since 2014, Abt has developed home health quality measures to rate the nearly 12,000 home health agencies certified by Medicare, and launched a star rating system on the Home Health Compare website to provide the public valuable information about the quality of home health care used by more than 5 million Americans annually. In addition, for the past 11 years, Abt has worked closely with CMS to develop, implement, refine, and support the Five-Star Quality Rating System for nursing homes that is part of the Nursing Home Compare website. These ratings allow patients and families to compare the quality of providers available in their area, as well as help home health agencies and nursing homes identify opportunities for quality improvement, and provide CMS with important quality information.
The nursing home Five-Star ratings measure nearly 16,000 nursing homes in the United States and are based on each nursing facility’s performance on annual health inspection surveys, staffing levels, and a set of quality measures. In recognition of the multi-dimensional nature of nursing home quality, the system includes ratings for each of these domains, along with an overall rating. Abt calculates nursing home ratings monthly, producing and delivering rating files for website display, along with a standard set of descriptive analytic reports on the ratings. Individualized “provider preview” reports are also generated so nursing home administrators can see their ratings prior to public reporting.
For the Medicare Home Health Quality Reporting Program, the Abt team also developed standardized, cross-setting measures in the important areas of medication reconciliation, potentially preventable hospitalizations, successful discharge to community, and transfer of health information, among others, as part of an initiative to enable comparing providers across the continuum of post-acute care. Ongoing monitoring of measures helps CMS and other stakeholders identify quality issues and measurement gaps.

Project Home Health Quality Reporting Program
Funder Centers for Medicare and Medicaid Services (CMS)
Quality through Hands-On Training
In Tanzania, the shortage of trained health care workers is a major barrier to improving the delivery of quality health services. Medical students studying at private training institutes have historically relied on practicum opportunities within public health facilities. These opportunities are limited, however, and many students have trouble getting the practical training needed to deliver quality essential health services.
In partnership with the Association of Private Health Colleges, Abt designed a pilot initiative to increase the practical clinical skills of nursing and midwifery students by engaging the private health sector. Fifty nursing and midwifery students rotated placements at private medical facilities affiliated with five major medical institutions in Tanzania. They received practical experience in FP, integrated HIV care, antenatal care, and primary health care. This pilot established an important new model for improving quality of service delivery by engaging the private sector to invest in the next generation of practitioners.
Project Sustaining Health Outcomes through the Private Sector Plus (SHOPS Plus)
Funder U.S. Agency for International Development (USAID)
Quality through Data Exchange
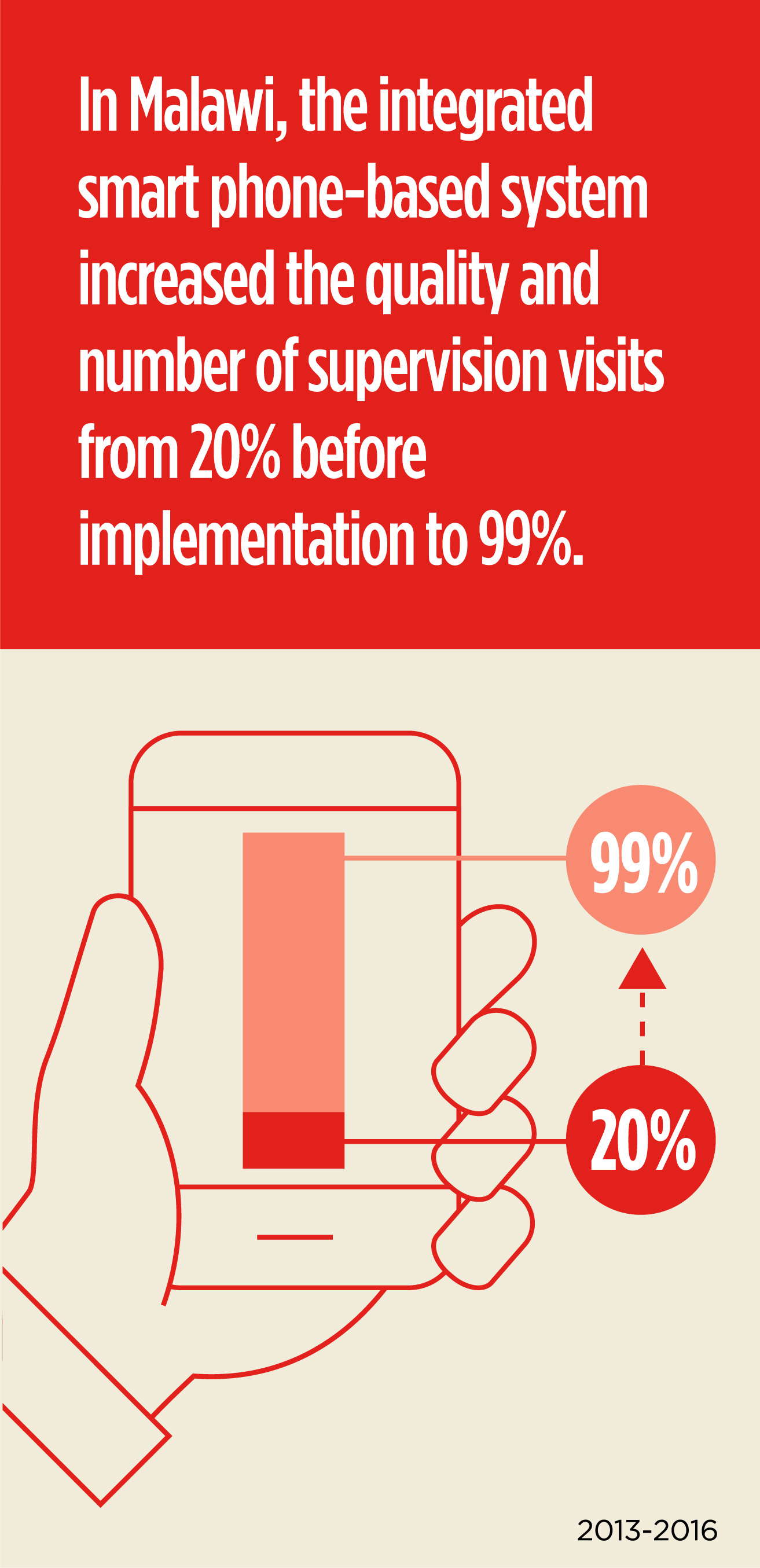
In Malawi, Abt helped build an integrated smart phone-based system that enables data on service quality to flow from even the most remote health centers across the country. Historically, the Ministry of Health relied on paper-based, siloed reporting systems focused on facility inspections. Now, the Ministry of Health is able to conduct regular supportive supervision visits and on-site coaching focused on health workers, increasing the quality and number of supervision visits from 20 percent before implementation to 99 percent. The electronic system allows for facility-level performance data to flow quickly to decision-makers, with results immediately available to their supervisors to support timely feedback and improvement steps. Supportive supervision visits powered by the integrated smart phone system facilitated improvements in service delivery, including increasing vaccination rates, ensuring proper installation of equipment, and streamlining systems that promptly unite babies with their mothers post cesarean-section.
Project Support for Service Delivery Integration—Systems (SSDI Systems)
Funder U.S. Agency for International Development (USAID)
In Tanzania, public service planning, budgeting, procurement, and reporting were previously conducted using separate systems for each function, making it difficult to manage resources appropriately. Additionally, planning and budgeting decisions were made at the national, regional, and local government levels, leaving individual facilities without autonomy to make decisions to meet their clients’ needs. The Abt-led USAID Public Sector Systems Strengthening (PS3) project has been working across sectors to improve health care and other essential public services, such as education and agriculture.
Working in close collaboration with government counterparts, the Abt team has developed management systems that are interoperable, allowing multiple functions to be completed through a single interface. Abt also supported the government’s efforts to link those systems to 25,000 health facilities and schools, and transition to output-based budgeting. This enabled health facility and school managers to make decisions that directly address the needs of their clients. Budget allocations are now visible in the system, improving the ability of facilities to procure medicine and other supplies. Interoperability is also improving drug procurement planning, as the central drug repository is able to monitor inventory across all facilities and prepare for procurement requests.
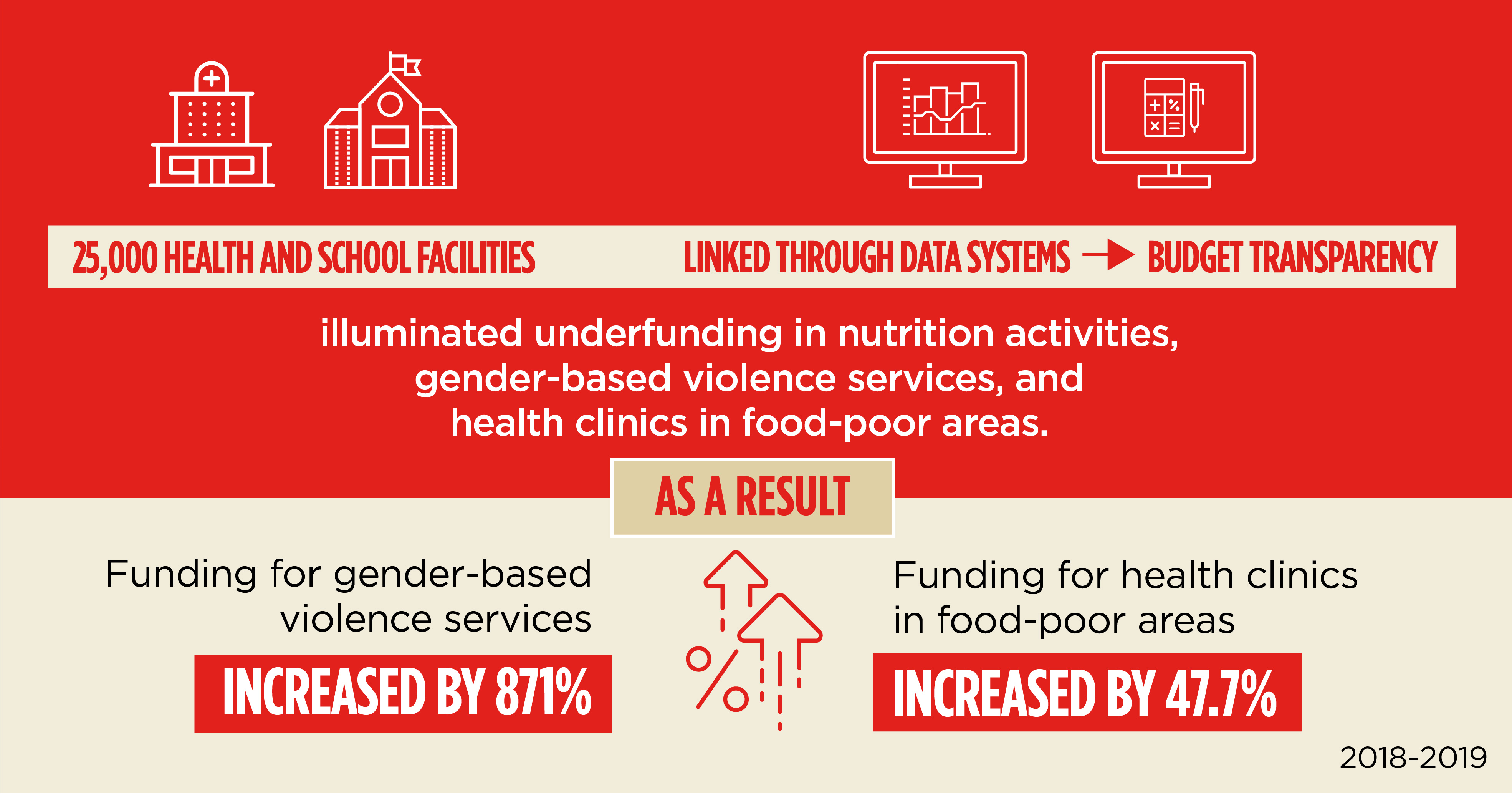
Extending the interoperable systems to the health facilities also created more budget transparency, facilitating the identification of priority areas that were not receiving their full allotment of funds. For example, nutrition services were found to be receiving TZS 16.7 billion, rather than the TZS 50 billion that had previously been estimated. Services for victims of gender-based violence were found to be substantially shortchanged and, as a result, funding for these services increased from TZS 0.34 billion in FY2018/19 to TZS 3.3 billion in FY2019/20—an 871 percent increase. Distribution of resources for health was reprioritized to vulnerable populations in food-poor areas, and in 2019, residents in food-poor areas received 47.7 percent more funding for health services.
Project Public Sector Systems Strengthening Activity (PS3)
Funder U.S. Agency for International Development (USAID)
