Opioid Misuse and Prevention


Since 2000, nearly 400,000 Americans lost their lives to the opioid epidemic. As the epidemic continues to reverberate through communities, it affects those with the opioid use disorder (OUD)—a chronic, recurring disease—as well as their families, friends, and local ecosystems of schools, employers, healthcare providers, and first responders.
It’s critical to understand that effective responses to the opioid epidemic go beyond the clinical health setting. Abt brings decades of interdisciplinary expertise in behavioral health, infectious disease, employment, housing, criminal justice, and child welfare to the fight against this epidemic. We have helped prevent opioid misuse and bolster social supports for recovery. We’ve developed and tested tools to improve opioid prescribing and evaluated the effectiveness of treatment programs. We apply a multidimensional lens to bring an end to this epidemic.
Generating the First National View of the Epidemic
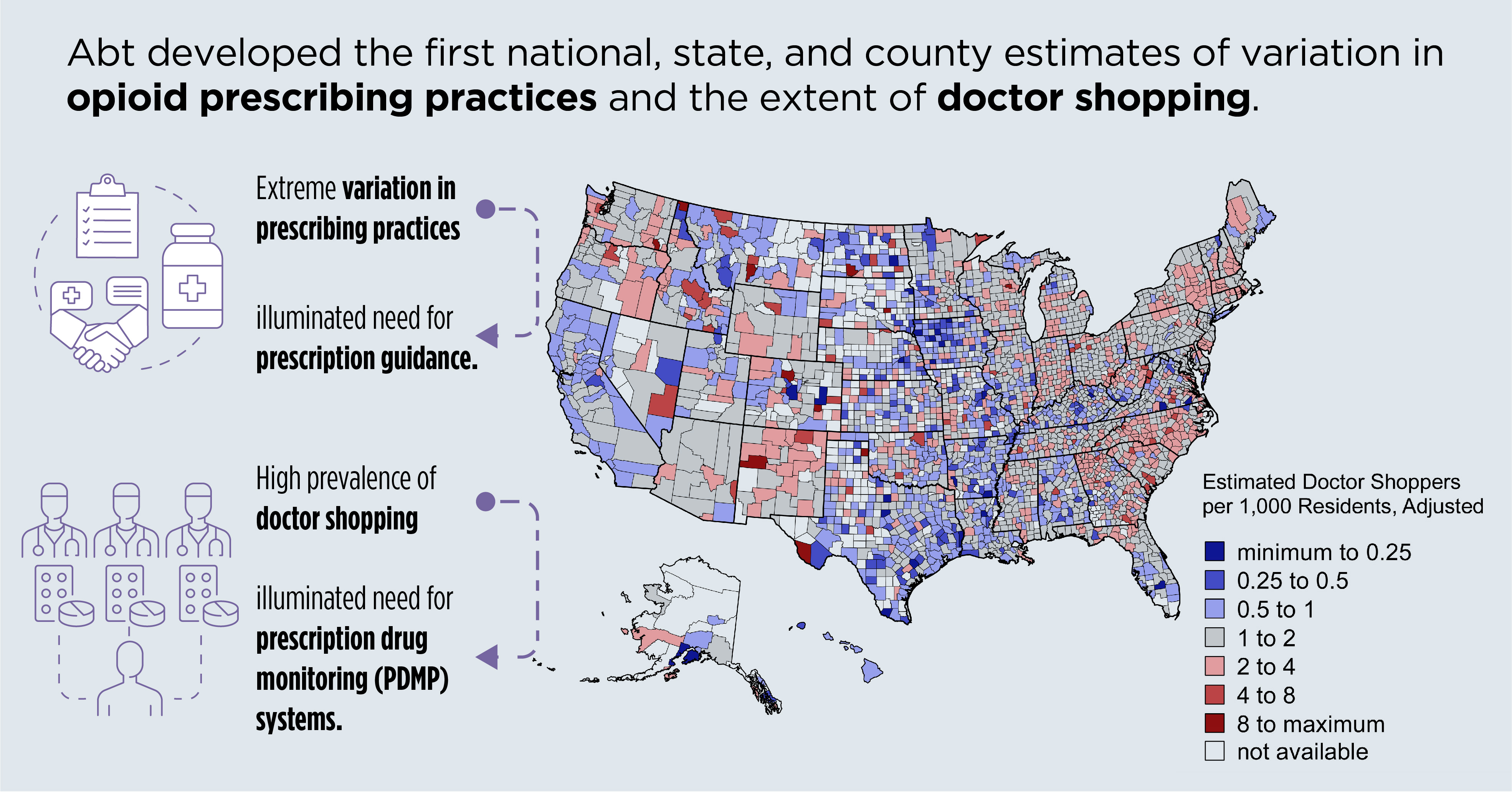
Abt developed the first national, state, and county estimates of the wide variation in prescribing practices for controlled opioid pain relievers. Evaluating more than 250 million prescriptions dispensed by retail pharmacies in the U.S. we found an extreme lack of uniformity in these practices—illuminating the need for better prescription guidelines.
Examining the same dataset, we developed the first national, state, and county estimates of the number of individuals “doctor shopping”—obtaining excessive amounts of opioids from multiple physicians who are unaware others are also prescribing to these patients. Documenting the prevalence of doctor shopping supported the case for investing in improved prescription drug monitoring systems.
Project Epidemiological Analysis of Rx Drug Use and Diversion
Funder National Institutes of Health/National Institute on Drug Abuse
Evaluating Effectiveness of Prescription Drug Monitoring Programs (PDMPs)
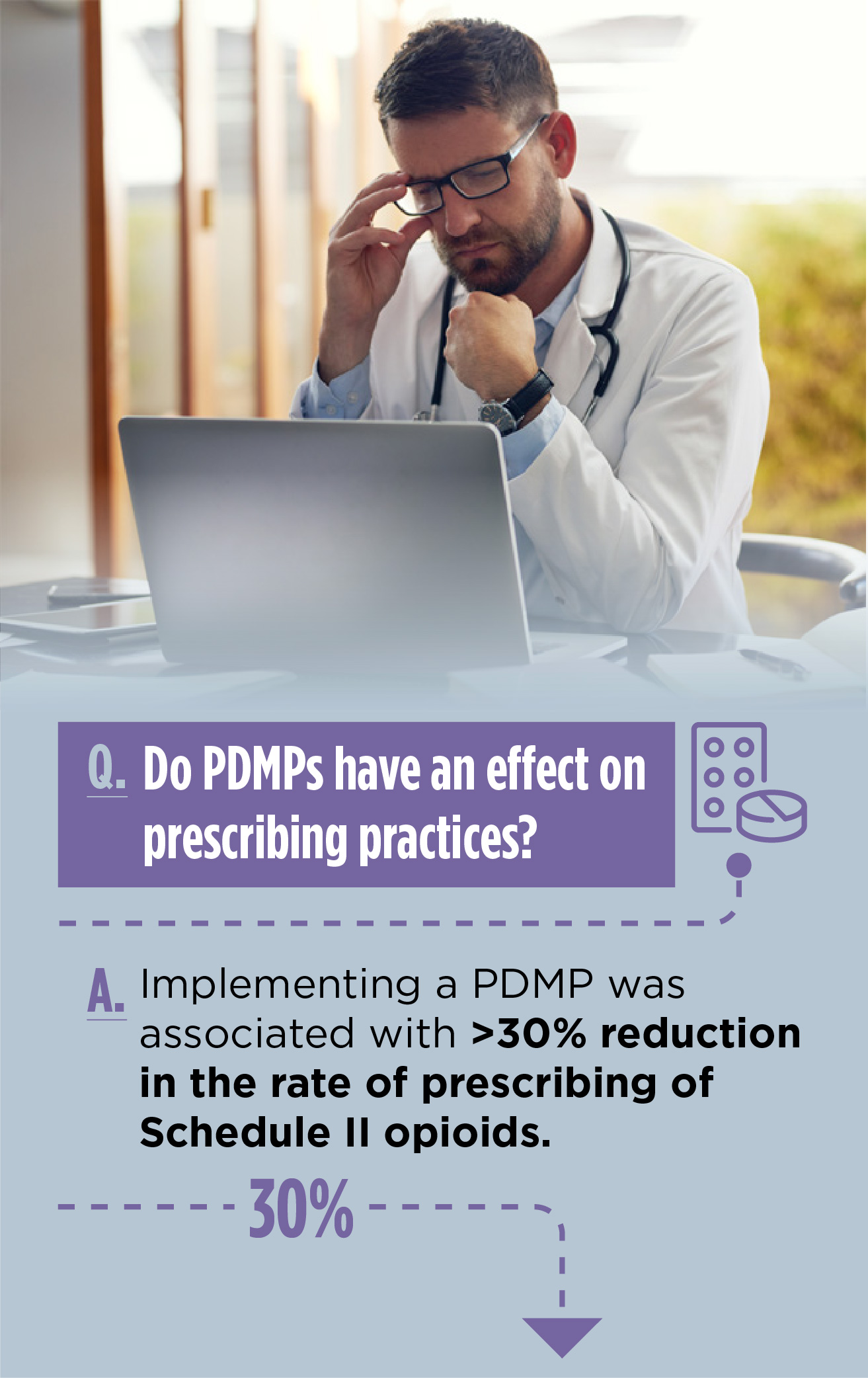
To combat doctor shopping and ensure coordinated care, many states have implemented Prescription Drug Monitoring Programs (PDMPs). Using an electronic database, a PDMP tracks information from pharmacies about all sales of controlled drugs within a state. Although PDMPs have the potential to assist prescribers in making informed decisions, their use varies widely.
Using national survey data spanning 24 states and 10 years, Abt researchers helped assess the beneficial effects of PDMPs on the prescribing of opioid analgesics and other pain medications in ambulatory care settings at the point of care.
Prescription Drug Monitoring Programs Are Associated With Sustained Reductions In Opioid Prescribing By Physicians. Yuhua Bao, Yijun Pan, Aryn Taylor, Sharmini Radakrishnan, Feijun Luo, Harold Alan Pincus, and Bruce R. Schackman. Health Affairs 2016 35:6, 1045-1051
Instead of relying on clinicians to access PDMP data, some PDMPs have used algorithms to flag patients whose purchasing patterns suggest misuse of controlled drugs. Some have also proactively notified these patients’ physicians and pharmacists with this information. Abt researchers conducted a random assignment experiment in Nevada to determine if such searches and proactive notification were effective in reducing patients’ ability to obtain large amounts of prescription opioids. They weren’t.
Project Field Experiment to Estimate Cost Effectiveness of Proactive Reporting by Prescription Drug Monitoring Programs
Funder Centers for Disease Control and Prevention (CDC)
Improving Clinical Practice
Guideline Development
To address the widespread inconsistencies in opioid prescribing practices, the U.S. Centers for Disease Control and Prevention (CDC) issued the Guideline for Prescribing Opioids for Chronic Pain. Abt supported CDC’s development of the Guideline by assessing the evidence base for all of the recommendations.
Project Support Development of Opioid Prescribing Guidelines
Funder Centers for Disease Control and Prevention (CDC)
Implementation and Quality Improvement (QI)
Guidelines are not self-executing and dissemination alone does not always make tough clinical decisions easier. To support implementation, Abt has worked with CDC on several initiatives focused on implementing the Guideline in health systems’ primary care practices.
One important contribution was the development of a resource for safe opioid prescribing that outlines the system-level changes needed to support clinical practice, in addition to clinical recommendations. For example, to further improve opioid prescribing, Abt and partners developed a set of 16 clinical quality improvement (QI) measures, aligned with the Guideline. These voluntary measures help healthcare systems understand their opioid prescribing practices and track progress toward fully implementing the Guideline over time as part of QI initiatives.
Project A Clinical Improvement Implementation Package for Large Healthcare Systems: Activities to Support Guideline Dissemination and Implementation
Funder Centers for Disease Control and Prevention (CDC)
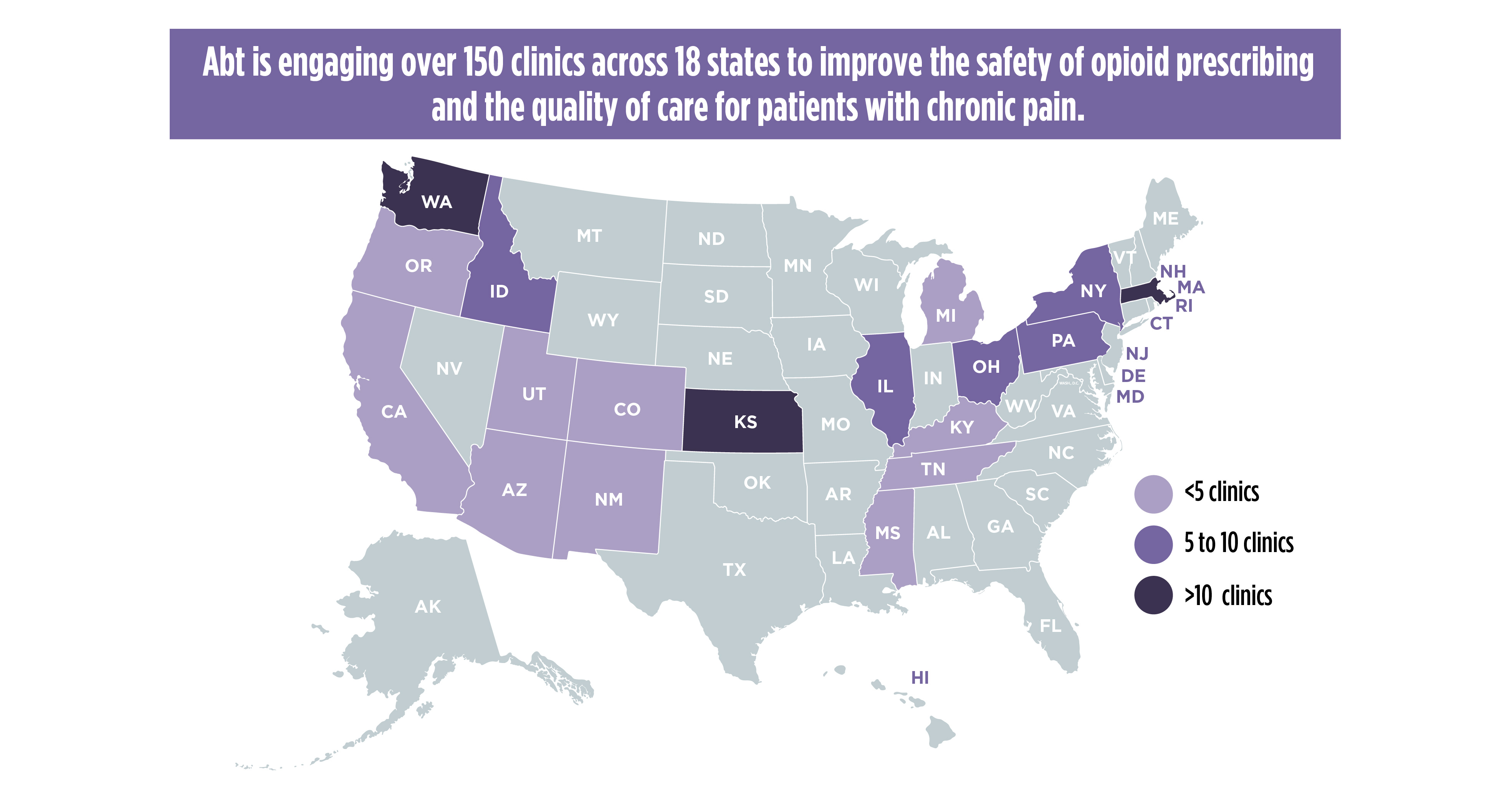
To further advance effective implementation of the Guideline and the associated QI measures, Abt facilitated the establishment and support of two cohorts of an opioid QI collaborative of health care systems seeking to implement the CDC Guideline, using the associated QI measures to monitor improvements over time and engage in shared learning. The collaborative includes two cohorts of healthcare systems across 11 states from Massachusetts to Oregon, and more than 120 primary care practices located in urban, rural, frontier, underserved, and tribal communities. Findings from the Collaborative have been presented at Academy Health 2018 and 2019 and the National Rx Abuse Summit in 2019 and 2020.
Project Implement and Evaluate CDC Opioid-Related Quality Improvement Measures in Clinical Settings
Funder Centers for Disease Control and Prevention (CDC)
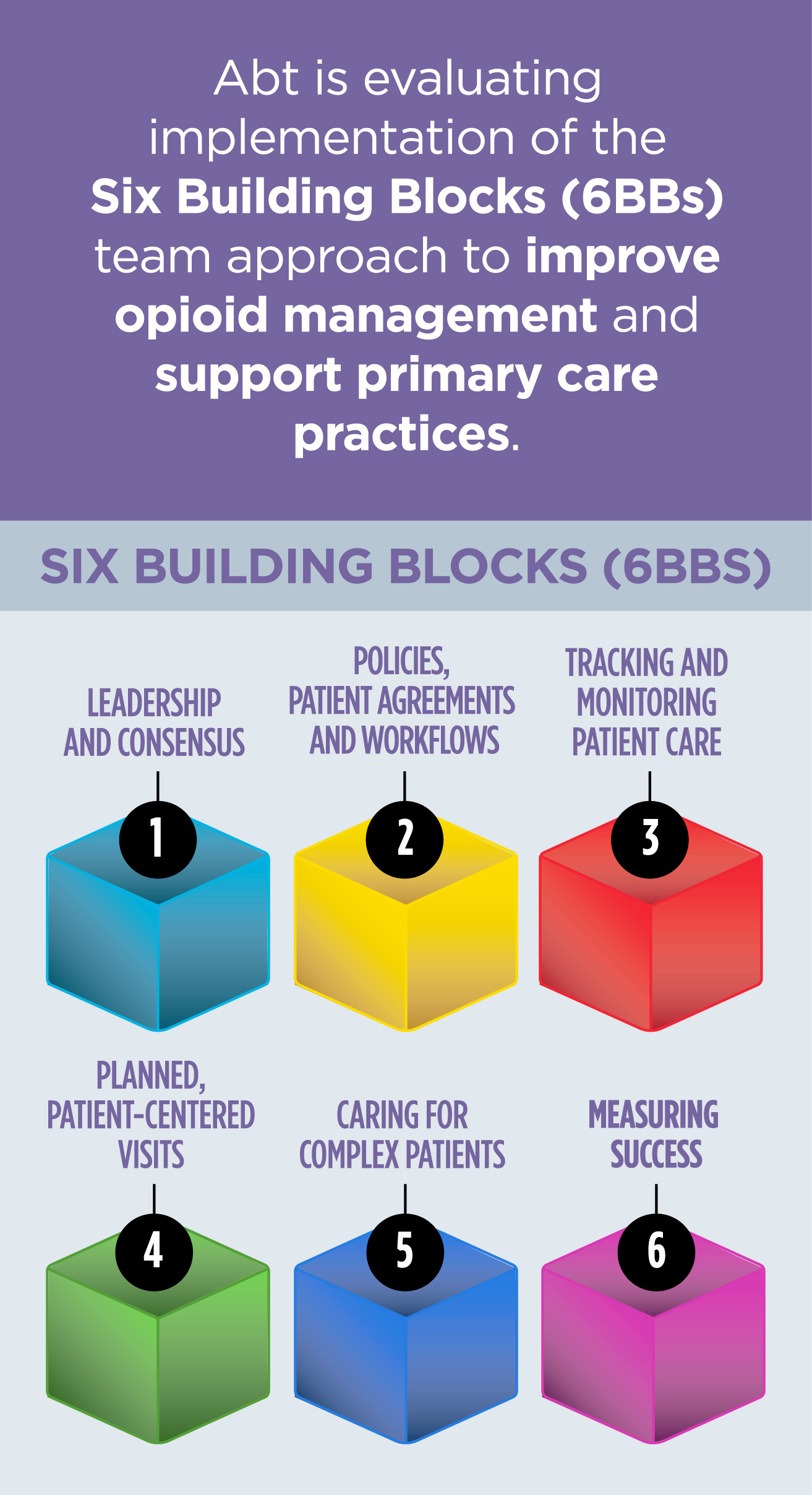
Abt is evaluating the implementation of the Six Building Blocks (6BBs) team approach to improve opioid management and support primary care practices. The 6BBs represent six key work areas that primary care practices need to redesign to improve management of patients on long-term opioid therapy. Abt and partners developed a 6BB Clinic Implementation Guide and recruited more than 40 primary care practices to use it. Participating practices span 10 states and include academic-affiliated clinics, federally qualified health centers, patient-centered medical homes, health-system or hospital-affiliated clinics, and private practices. See the recently-published evaluation protocol for this study.
Project: Evaluating and Implementing the Six Building Blocks Team Approach to Improve Opioid Management in Primary Care
Funder: Agency for Healthcare Research and Quality (AHRQ)
Harnessing Technology
To empower clinicians with guidance and resources at the point of patient care, Abt developed, implemented, and evaluated electronic clinical decision support (CDS) tools for pain management and opioid prescribing. CDS tools are integrated into the electronic medical records and enable prescribers to receive alerts suggesting best practices. They include developing opioid treatment agreements with patients, automated order sets, cautions about co-prescribing contraindicated medications, checking PDMP data, and referrals for treatment of opioid use disorders. The CDS tools were developed, implemented, and evaluated in four large healthcare systems serving as pilot sites and will be made available to other systems for adoption. Findings from the project were presented at American Public Health Association (APHA) 2019.
Project CDC Opioid Prescribing Guideline Implementation: Developing and Evaluating an Electronic Clinical Decision Support System
Funder Centers for Disease Control and Prevention (CDC)
Opioid treatment is vulnerable to both unplanned service disruptions, such as natural disasters, and planned ones, like travel. Abt evaluated a Substance Abuse and Mental Health Services Administration (SAMHSA) health pilot project that supported continuity of care by enabling patients to control the sharing of their opioid treatment information with other providers via a Health Information Exchange and a patient portal. Our analysis detailed the challenges associated with developing the solution, the extent to which SAMHSA’s goals for this pilot were met, lessons learned, and recommendations for future applications of these findings.
Project Opioid Treatment Program Service Continuity Project
Funder FEi and Substance Abuse and Mental Health Services Administration (SAMHSA)
Abt led the development of a text messaging library for SAMHSA to support individuals with OUD. Informed by stakeholder and expert interviews, Abt developed and tested 150 text messages targeted to individuals in various stages of recovery and developed supporting implementation materials for the library.
Project Behavioral Health Information Technologies and Standards (BHITS)
Funder Substance Abuse and Mental Health Services Administration (SAMHSA)
Addressing Prevention, Treatment, and Recovery in Communities and Systems
Effectively combating the opioid epidemic requires a response beyond the clinical setting. It depends on collaboration across the public health sector and broader community and a deep understanding of determinants of recovery.
For the U.S. Department of Health and Human Services, Abt supported the development of the first-ever Surgeon General’s Report on Alcohol, Drugs, and Health. This seminal publication serves as a definitive resource for how the U.S. approaches not only opioid misuse but also public health problems associated with alcohol and other substances.
Project: Surgeon General’s Report on Alcohol, Drugs, and Health
Funder: Substance Abuse and Mental Health Services Administration (SAMHSA)
Bringing a Multidimensional Recovery Lens
The impacts of opioid use and misuse affect every aspect of a person’s life— employment, housing, and children, among others. Abt’s multidimensional approach includes working with communities and partners on the social determinants that encourage healing.
To identify housing solutions that support recovery from OUD, Abt conducted a detailed literature review on the subject, as well as an environmental scan and interviews with experts and providers. Our research identified several promising strategies as well as gaps in knowledge to help guide future research. Additionally, the study of housing models will help local jurisdictions scale up and evaluate effective programs.

Project Opioid Use Disorder, Housing Instability, and Housing Options for Recovery
Funder U.S. Department of Health and Human Services (HHS), Office of the Assistant Secretary for Planning and Evaluation (ASPE)