HIV & AIDS


Since it began nearly 40 years ago, the AIDS epidemic has claimed more than 32 million lives. With breakthroughs in detection, treatment, and de-stigmatization, the possibility of an AIDS-free generation is drawing closer. Yet even as global goals aim to control 95 percent of the epidemic by 2030, the pace of progress is slowing down. Some countries are experiencing rises in new HIV infections and AIDS-related deaths. To finally end the AIDS epidemic, it is critical that efforts reach the most marginalized, use evidence of what works, and build local capacity to effectively take on the fight as donor funding shrinks.
Abt started to combat HIV/AIDS in 1987. Since then, we have advanced knowledge about prevention, detection, and care in the U.S. and around the world. We have expanded access to testing, care, and treatment. We have strengthened health systems to provide quality services in the U.S. and in more than 20 high-burden HIV countries. We have integrated the private sector into these efforts. And we have built capacity for sustainably funding interventions that improve the quality of life for those living with the disease.
Bringing Countries Closer to Self-Reliance in Stopping the Epidemic
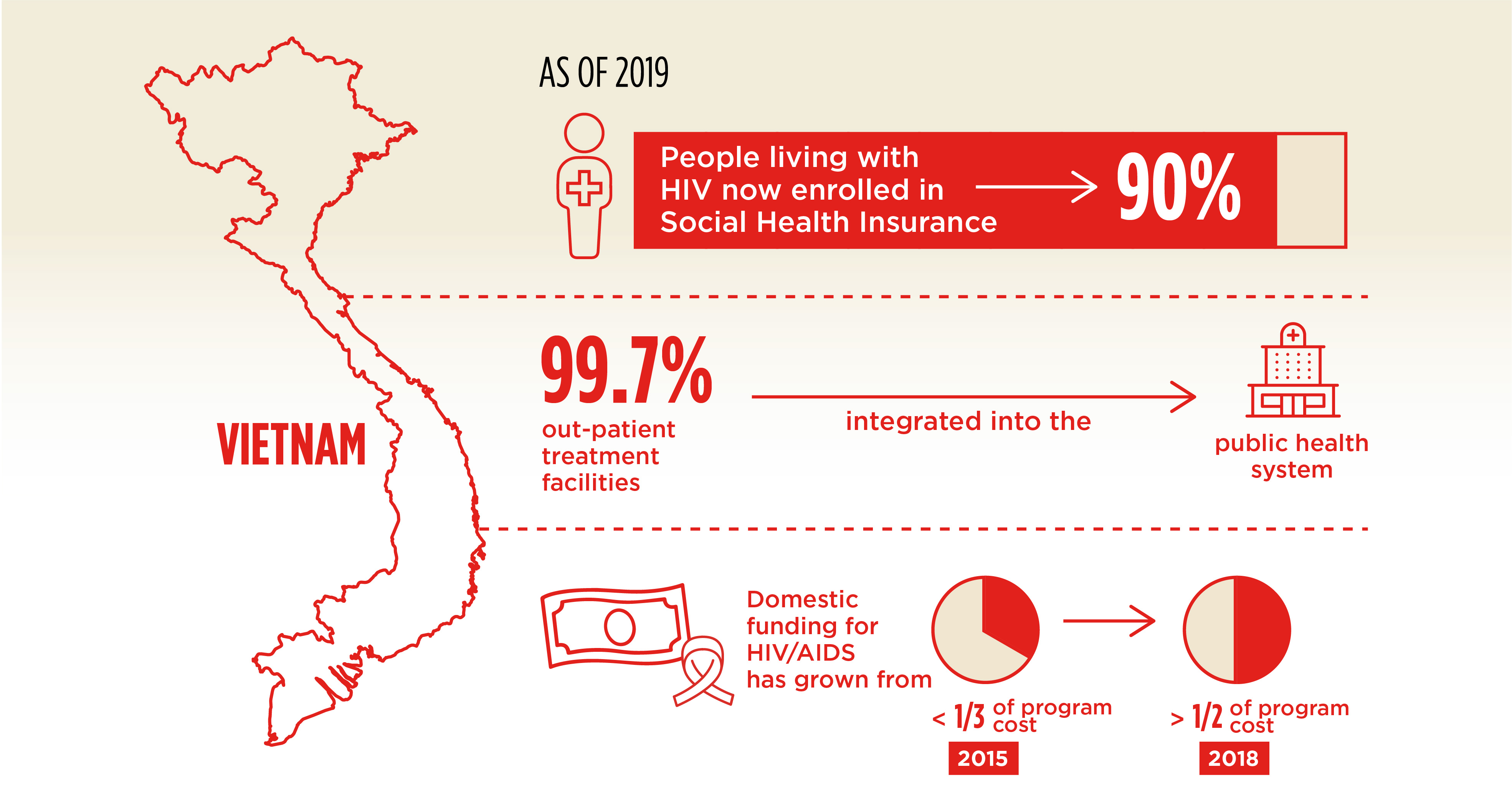
By 2014, Vietnam had made significant progress in the prevention and treatment of HIV/AIDS, primarily due to substantial financial contributions from international donors. The contributions funded more than 70 percent of the country’s HIV/AIDS response. With the donors’ planned withdrawal looming, financial sustainability of HIV/AIDS services became a top priority.
Abt worked with the Government of Vietnam to manage the transition from donor funding to a domestically financed HIV response. We partnered with government agencies to add HIV/AIDS services to the country’s social health insurance (SHI) scheme. We helped centralize procurement of antiretroviral (ARV) drugs and integrate HIV outpatient facilities into the public health system so that they would be eligible for SHI reimbursement. An early projection estimated that SHI coverage of 52 percent of people living with HIV by 2022 would avert more than 2,500 deaths.
As Abt continues to work with the government of Vietnam, progress has already outpaced past projections. As of 2019, the percentage of people living with HIV enrolled in SHI has reached 90 percent. Copayments and premiums are subsidized to provide financial protection to the most vulnerable groups, and 99.7 percent of the country’s out-patient treatment facilities have been integrated into the public health system. In addition, domestic funding for HIV/AIDS has grown from covering less than a third of the program to covering more than half in 2019.
Project Health Finance and Governance (HFG); USAID Sustainable Financing for HIV
Funder U.S. Agency for International Development (USAID)
Most of the Dominican Republic’s (DR) estimated 67,000 people living with HIV (PLHIV) are from high-risk groups. They include, men who have sex with men (MSM), female sex workers, transgender individuals, and migrants. About 12,000 of them receive HIV prevention and treatment services from non-governmental organizations (NGOs) funded by the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR). Abt is working to strengthen these NGOs and help them gain new revenue sources, including accessing insurance payments. A critical step to ensure the NGOs’ sustainability is to enable NGOs to contract with Seguro Nacional de Salud (SENASA), the public health insurance company. Then they could receive payment for providing HIV and primary care services to PLHIV enrolled in the insurance scheme. Abt’s work includes advocating to SENASA to pursue contracts with NGOs and helping NGO partners navigate SENASA’s contracting requirements. We also work with the NGOs and government to develop a strategy to increase enrollment of PLHIV.
Project Sustaining Health Outcomes through the Private Sector Plus (SHOPS Plus)
Funder U.S. Agency for International Development (USAID)
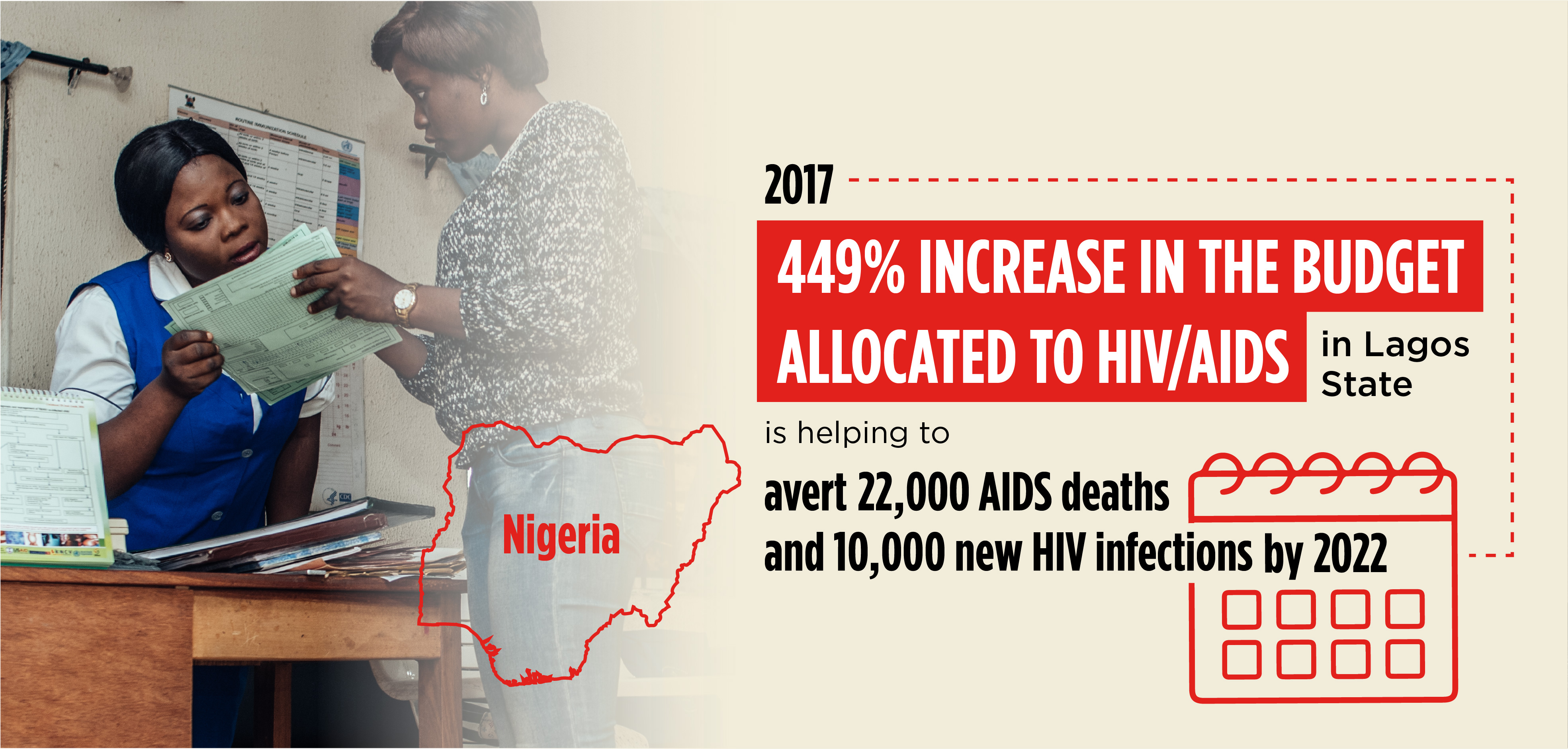
Nigeria’s oil wealth catapulted its economy to be the largest in Africa in 2017. Yet its expenditure on health continued to be very low, representing only 4 percent of the 2018 annual budget. External donors funded 70 percent of Nigeria’s HIV/AIDS response. Abt’s work in Nigeria focused on increasing domestic resources for HIV programs. In Lagos State—the country’s economic engine and the most densely populated of Nigeria’s states—Abt supported the AIDS Control Agency in advocating for state financing of HIV/AIDS programs. We assisted with resource tracking analyses, advocacy briefs, political economy analyses, and advocacy meetings with legislators and the Ministry of Finance. The resource tracking analyses followed the flow of health-sector funds from public, private, individual, and donor sources to their end uses. It developed the evidence needed to raise awareness of Lagos State’s low public spending on HIV/AIDS and the over-reliance on external funding. As a result of these advocacy efforts, Lagos State achieved a 449 percent increase in the budget allocated to HIV/AIDS in 2017. The significant increase in domestic investment that Abt successfully facilitated is projected to avert 22,000 AIDS deaths and 10,000 new HIV infections by 2022.
Project Health Finance and Governance (HFG)
Funder U.S. Agency for International Development (USAID)
Improving Public Sector Efficiency
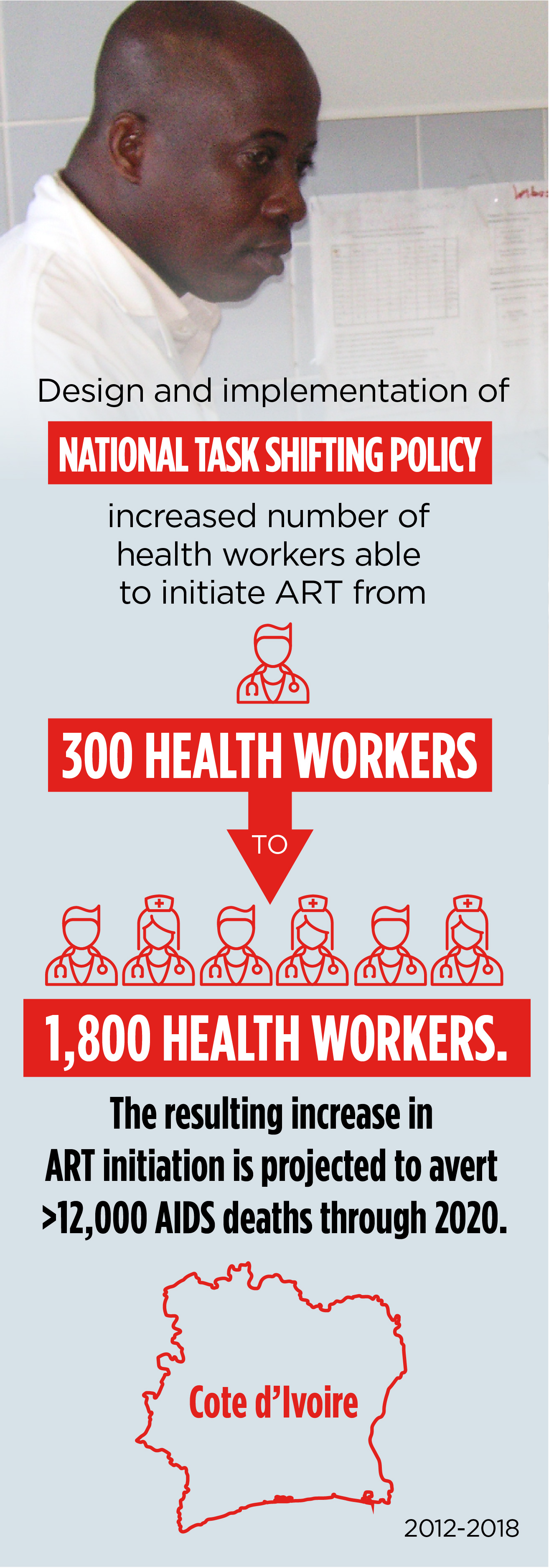
Since 1995, Abt has been working to strengthen the health system of Cote d’Ivoire, a country with one of the highest HIV prevalence rates in West Africa. Since the late 90s, the country has seen steady progress in the reduction of HIV prevalence. Yet in 2013, that prevalence was still at 3.2 percent, below the rate for Africa but four times the global average. And more than 50% of HIV positive adults and children had yet to receive ART.
One challenge was an extreme shortage of skilled health workers able to provide ART services, as only physicians were allowed to administer HIV care. Another was that providers were clustered around Abidjan, Cote d’Ivoire’s largest city, leaving thousands of adults and children without life-saving HIV treatment.
Abt collaborated with the Ivorian Ministry of Health and Public Hygiene, local professional associations, and other partners to develop and promote adoption of a national task shifting policy that enabled nurses and midwives to provide critical ART services. We designed and implemented an education program to ensure high quality of care. We also facilitated the allocation of the new providers to districts experiencing the highest burden of HIV.
Between 2013 and 2018, Abt partnered with the Ivorian government to facilitate finance and governance transformations which have led to increased resources and better financial management. For example, we successfully advocated for an increase in domestic spending for HIV/AIDS commodities. This resulted in a 400 percent budgetary increase in 2017 over the previous year.
Project Health Finance and Governance (HFG)
Funder U.S. Agency for International Development (USAID)
Engaging the Private Sector
Engaging the private sector in the fight against HIV/AIDS has transformed Cote d’Ivoire’s response to the epidemic, and Abt has facilitated that transformation. An assessment that Abt conducted in 2013 found that the private health sector, which represents approximately 50 percent of the health care facilities in the country, was not sufficiently engaged in HIV service delivery. We also found that beyond offering an opportunity to expand access to care, the private sector could play a role in addressing the stigma and confidentiality issues that make some people reluctant to seek care in the public sector.
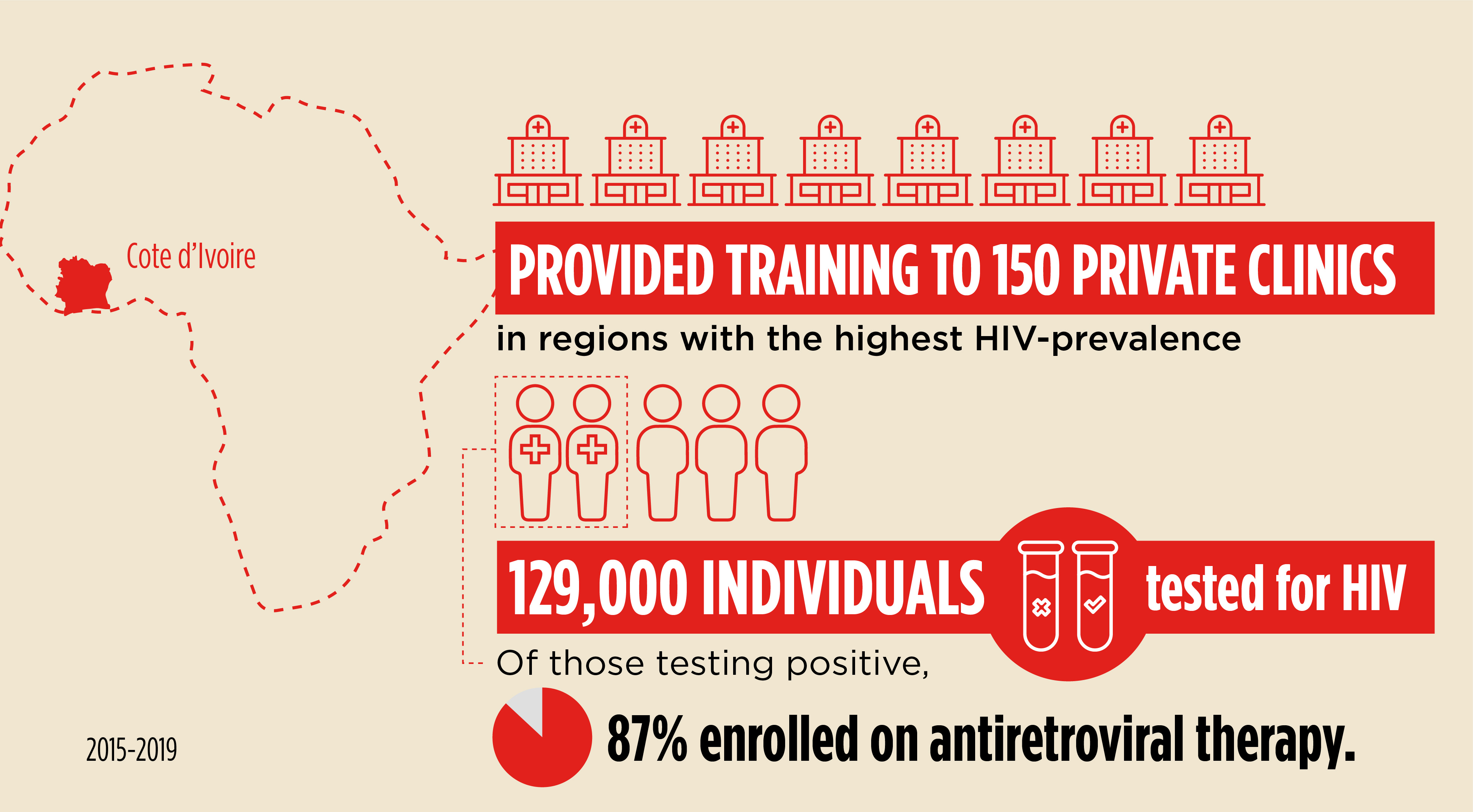
Abt led a four-year USAID program to expand the provision of quality HIV care, prevention, and treatment services—including access to ART. We created the first private network of HIV care and treatment sites in Cote d’Ivoire and linked it to the health system at the national, regional, and district levels. For the first time in Cote d’Ivoire, private sector patients now have access to HIV care consistent with national policies and guidelines. Private sector HIV data is regularly reported into the national system. And HIV activities are coordinated across the public and private sectors through leadership from the district-level health authorities.
Project Private Sector Health Project (PSHP)
Funder U.S. Agency for International Development (USAID)
Corporate Partnership increases access to HIV services for transport workers
Mobile populations, and particularly workers employed in the transport industry, are particularly vulnerable to HIV/AIDS. In Tanzania, Abt strengthened a private sector partnership to improve the sustainability of the HIV response by addressing health challenges facing transport workers specifically. Partnering with North Star Alliance—a social enterprise bringing care to transport workers and the surrounding communities through roadside wellness clinics—Abt helped register six North Star Alliance clinics with the ministry of health and the Private Hospital Advisory Board and trained their providers on an expanded set of HIV services. As a result, the clinics were able to establish formal relationships with public facilities for referrals, access to antiretroviral medicines, and data sharing. In 2019, the clinics tested more than 3,000 people for HIV and helped all who tested positive enroll into care.

Project Strengthening Health Outcomes through the Private Sector Plus (SHOPS Plus)
Funder U.S. Agency for International Development (USAID)
In Ethiopia, Abt has partnered with the Ministry of Health for more than 20 years. Our work to increase private sector engagement in the country’s HIV response is one of our most important contributions to improving the health of Ethiopians.
Though private facilities in Ethiopia were permitted to provide screening, counseling, and treatment for HIV and AIDS, they lacked access to funds to scale and invest in effectiveness. In 2011, USAID signed a 10-year Development Credit Authority (DCA) guarantee with two Ethiopian banks to expand HIV and AIDS services—the first such guarantee under PEPFAR. Abt worked with banks to broaden private health providers’ access to the funds and support emerging private sector models via technical assistance. With Abt’s assistance, 241 private providers received DCA lending to expand facilities, purchase new equipment, and increase working capital. Between 2015 and 2018, Abt’s efforts increased access to HIV services for 52,358 individuals. Facilities with DCA loans showed an increase of 31% in the number of HIV-affected patients served, and a 151 percent increase in the overall number of patients.
Separately, Abt is continuing to scale the capacity of private facilities to provide high-quality HIV and tuberculosis care. Through Abt’s support to private facilities, HIV testing services have been provided to nearly 761,000 clients and comprehensive ART services have been delivered to more than 8,700 people living with HIV.
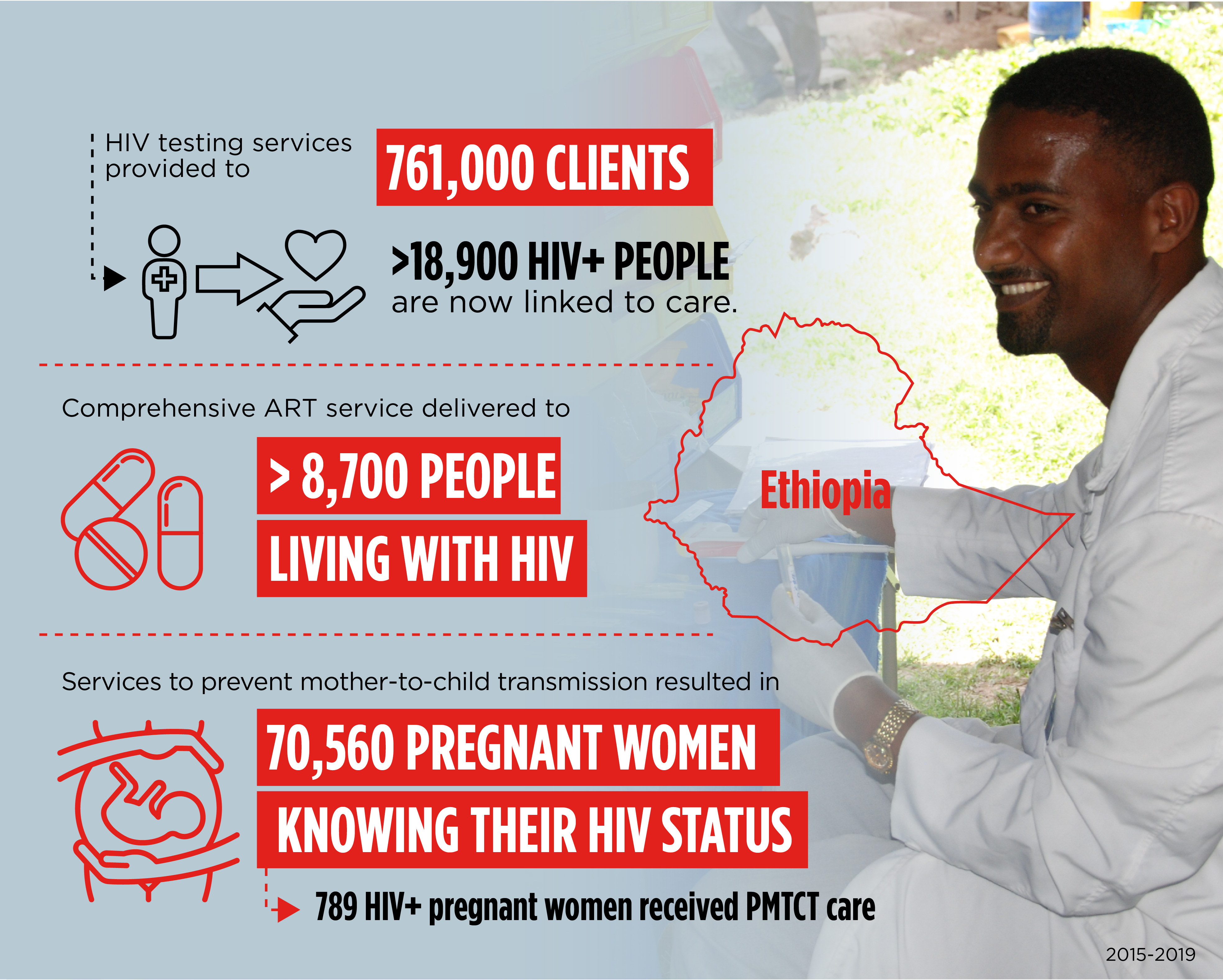
Project Strengthening Health Outcomes through the Private Sector Plus (SHOPS Plus) and Ethiopia Private Health Sector Project (PHSP)
Funder U.S. Agency for International Development (USAID)
Reaching the Most Vulnerable and Ensuring Treatment Adherence
In the U.S., we are improving the continuum of HIV care for the most vulnerable populations. For example, in three Massachusetts communities, we are increasing HIV primary care retention and viral load suppression rates among those hardest to reach: HIV+ women of color, MSM, and youth over 18 transitioning out of care.
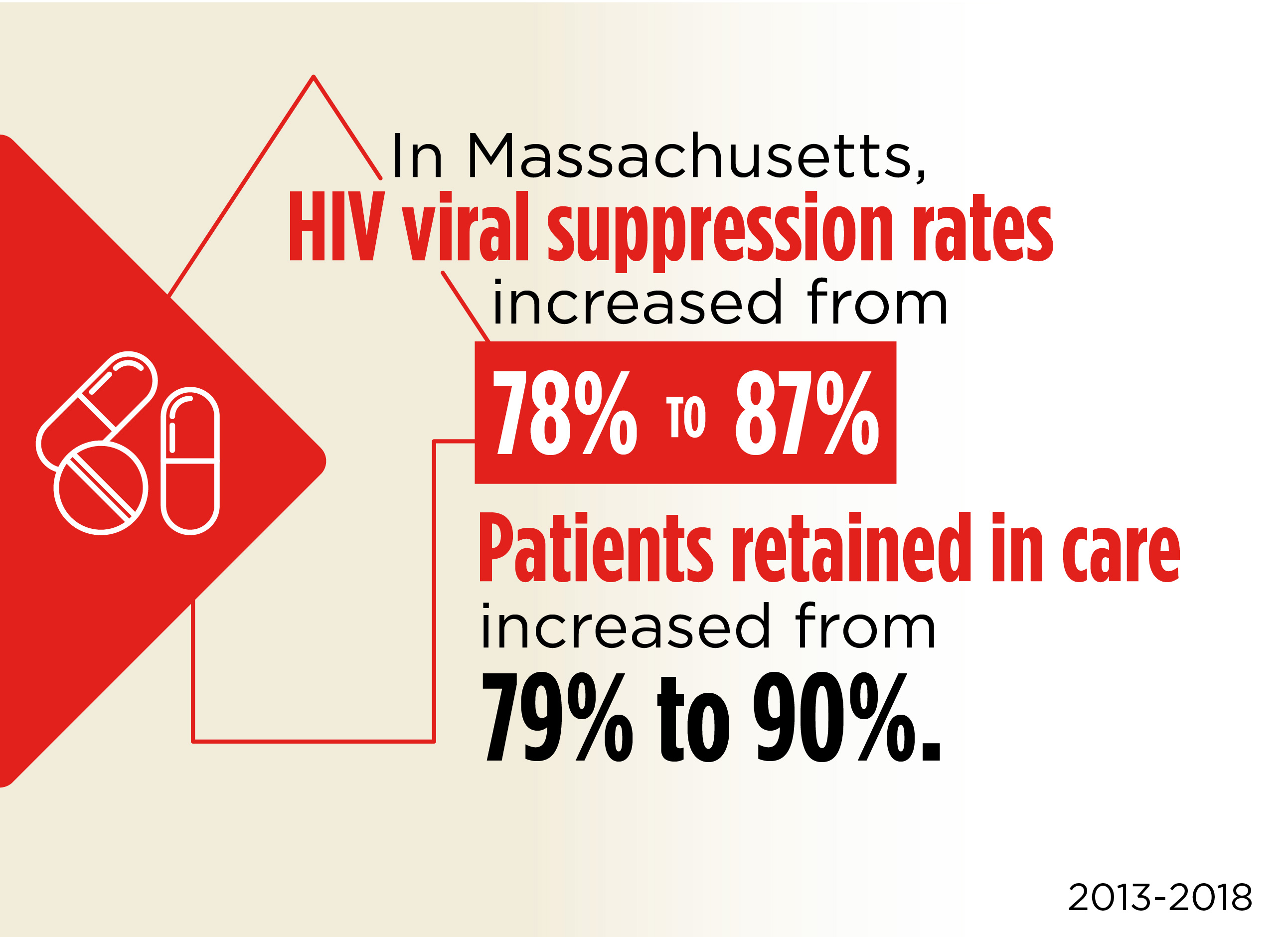
Project Consumer Access and Adherence to Care for HIV (CAATCH), Ryan White HIV/AIDS Program
Funder Health Resources and Services Administration (HRSA)
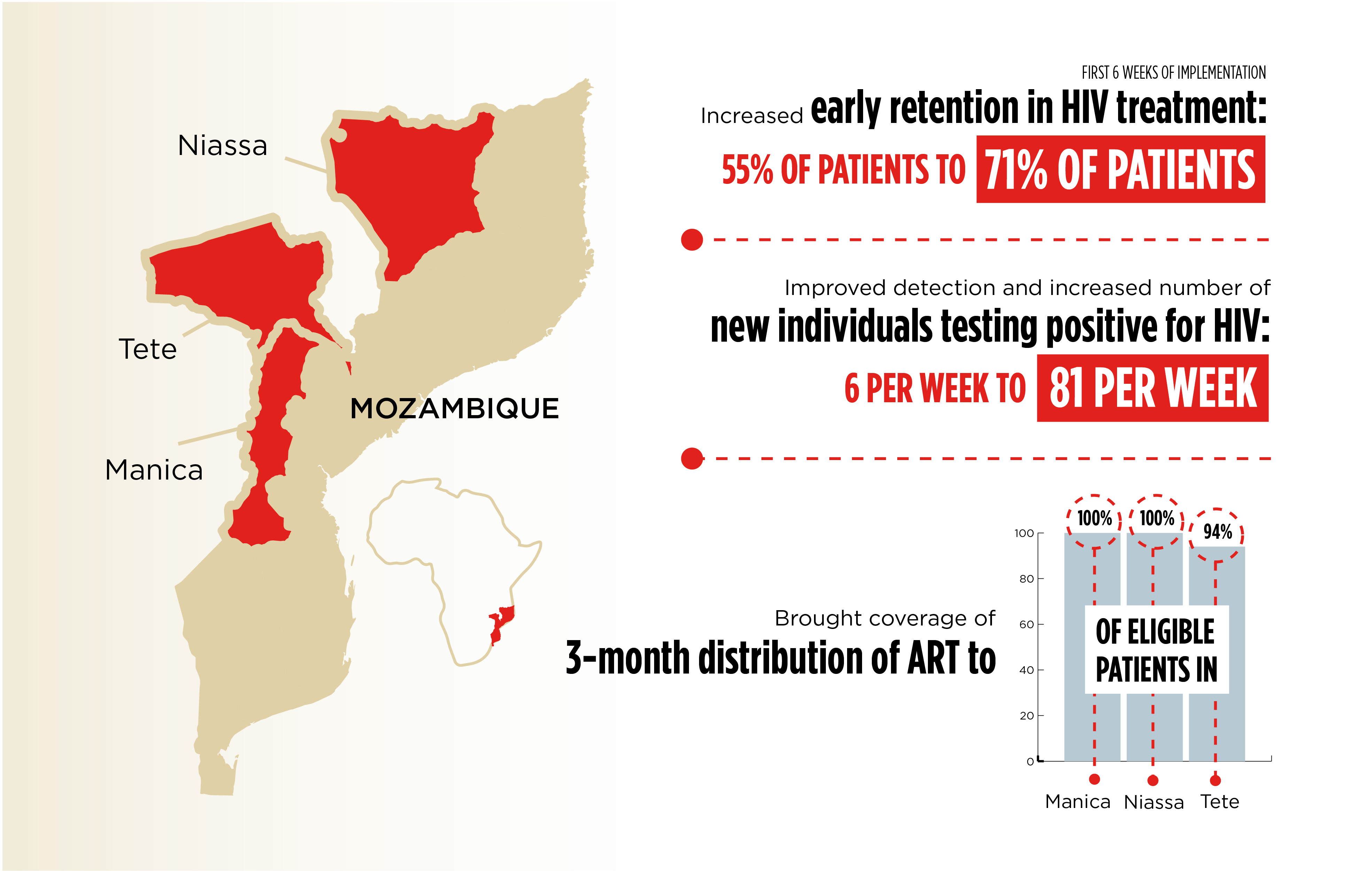
Abt has been supporting USAID’s and PEPFAR’s investments in fighting the HIV epidemic in Mozambique since 2010. Tasked with pivoting the HIV/AIDS response from an emergency response to one focused on improved sustainability, we focused on HIV clinical services in the central provinces of Sofala, Manica, and Tete. By implementing a district-focused approach and providing technical and material assistance, we strengthened the health system’s institutional capacity to provide high-quality services. We improved integration of HIV and primary health care services. And we increased demand and provision of high-quality HIV services, coverage of HIV care and treatment, and prevention of mother-to-child transmission services.
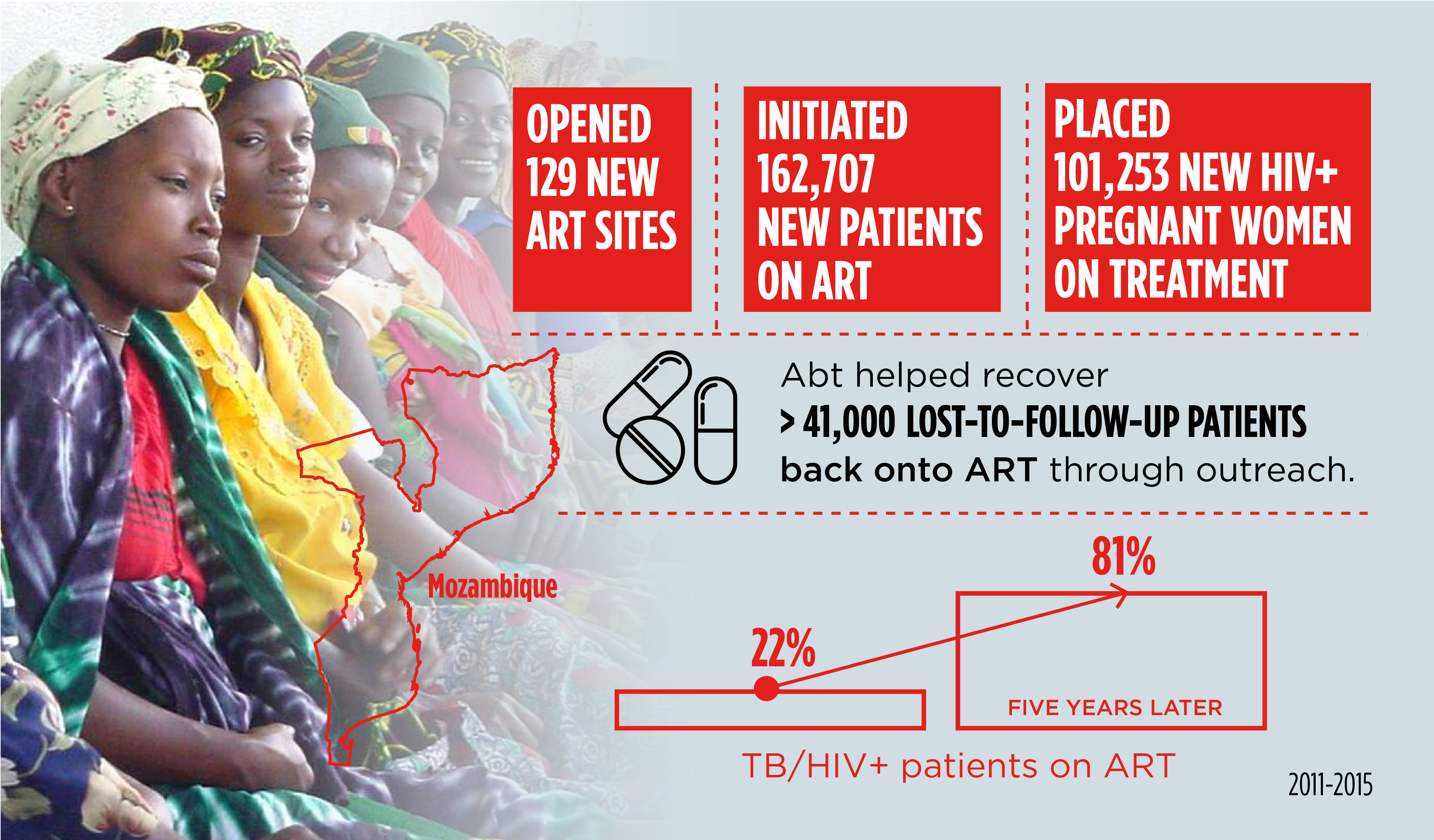
Abt is now expanding on this work, also with USAID/PEPFAR funding, to support the Government of Mozambique in achieving epidemic control in Sofala, Manica, Tete, and Niassa provinces by 2024. Under Abt’s leadership, this new initiative is off to a promising start.
Project Clinical HIV/AIDS Services Strengthening Project in Sofala, Manica, and Tete (CHASS SMT); Efficiencies for Clinical HIV Outcomes (ECHO)
Funder U.S. Agency for international Development (USAID)
Strengthening Government Response in the United States
The U.S. government announced a commitment to end the country’s HIV epidemic by 2030. To meet this ambitious goal, the government must base diagnosis, treatment, and prevention programs on rigorous evaluations and the best implementation science—disciplines Abt has been advancing for more than three decades.
Strengthening the Ryan White HIV/AIDS Program
The Ryan White HIV/AIDS Program (RWHAP), administered by the U.S. Health Resources and Services Administration, provides a comprehensive system of care for people living with HIV/AIDS, and targets populations disproportionately impacted by the epidemic.

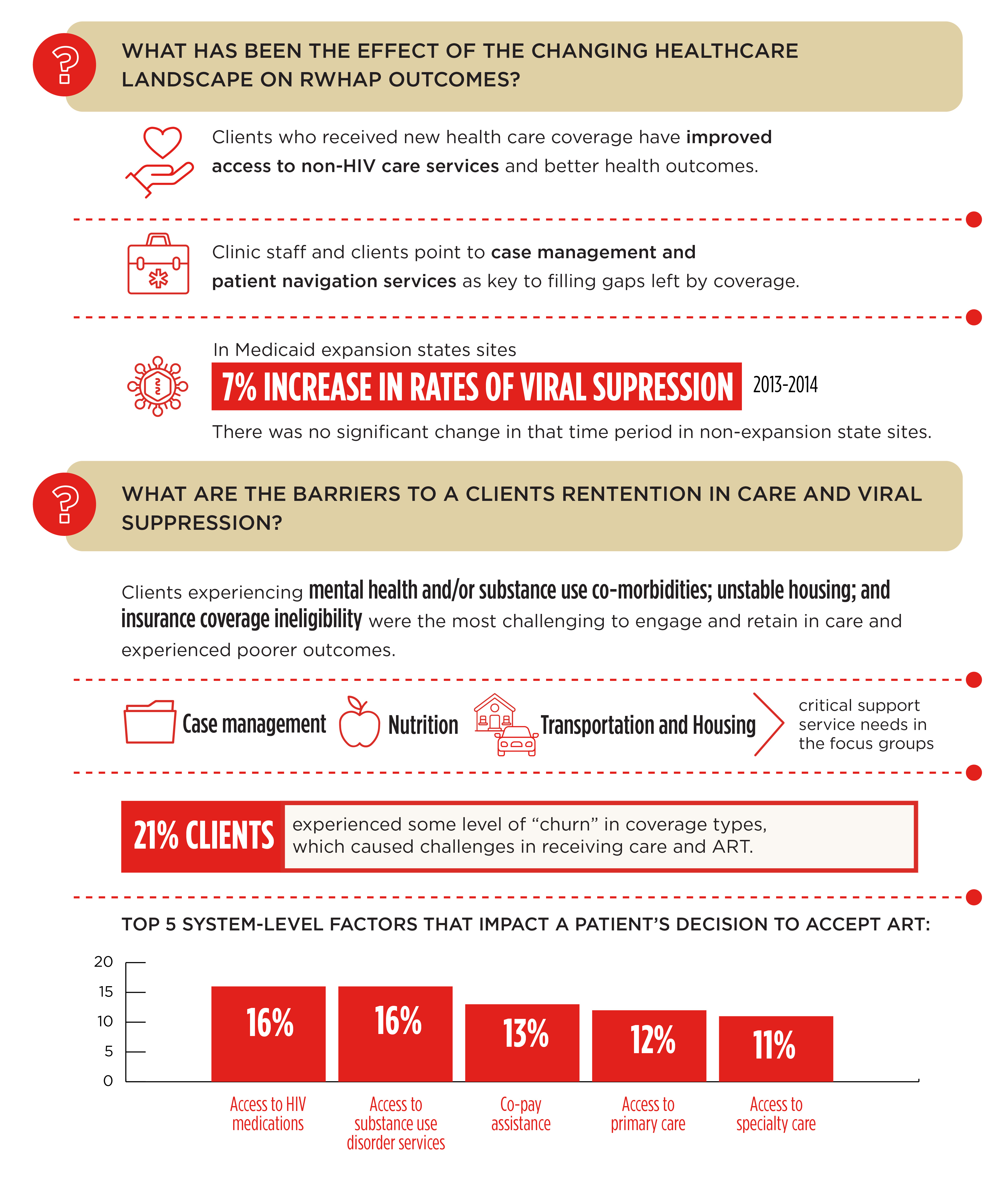
To strengthen RWHAP’s effectiveness and reach, Abt has furthered the understanding of barriers to care and to maintaining viral suppression and the unmet needs of these vulnerable populations.
Implications of the Changing Health Care Landscape
Since 2012, Abt has been conducting outcome studies to help RWHAP become even more effective. The passage of the Affordable Care Act represented a major change within the U.S. health care system and has potentially major implications for patients’ ability to access needed care.
Abt conducted a mixed-methods study that included interviews with more than 30 Ryan White-funded provider sites and analyzed Ryan White program- and client-level data to observe changes in insurance uptake and service utilization patterns. There main questions were as follows.
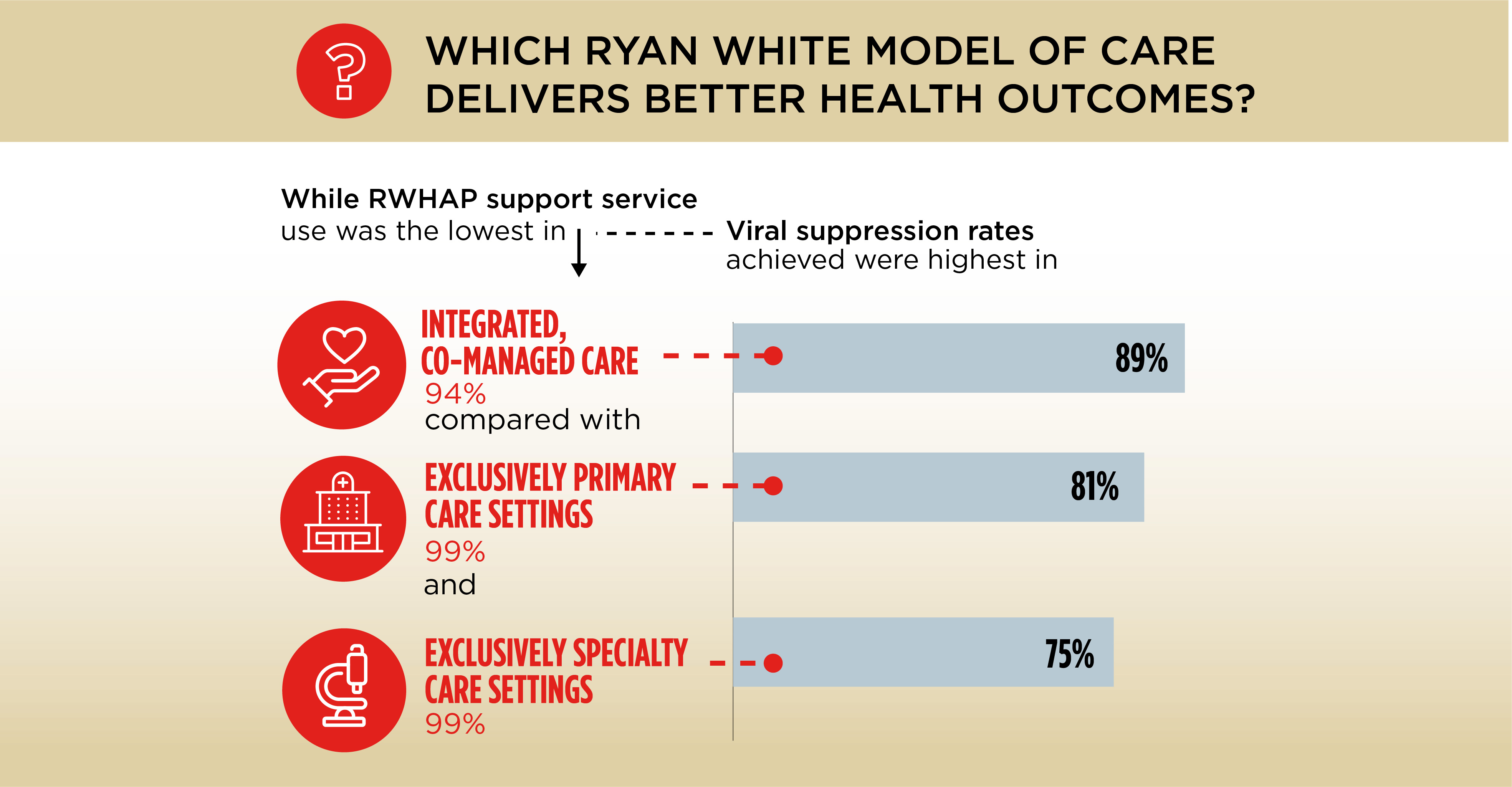
Effectiveness of RWHAP Healthcare Delivery Models
Although RWHAP clients have better clinical outcomes than those outside the program, little is known about how the model of healthcare delivery contributes to these outcomes. RWHAP providers generally follow three models of care: primary, specialist, and integrated, with varying use of RWHAP support services. The Abt study team used a retrospective case-control study to compare HIV and primary health care outcomes in each of the three models. The final analysis, which included more than 1,000 client observations from 70 sites, answered the question:
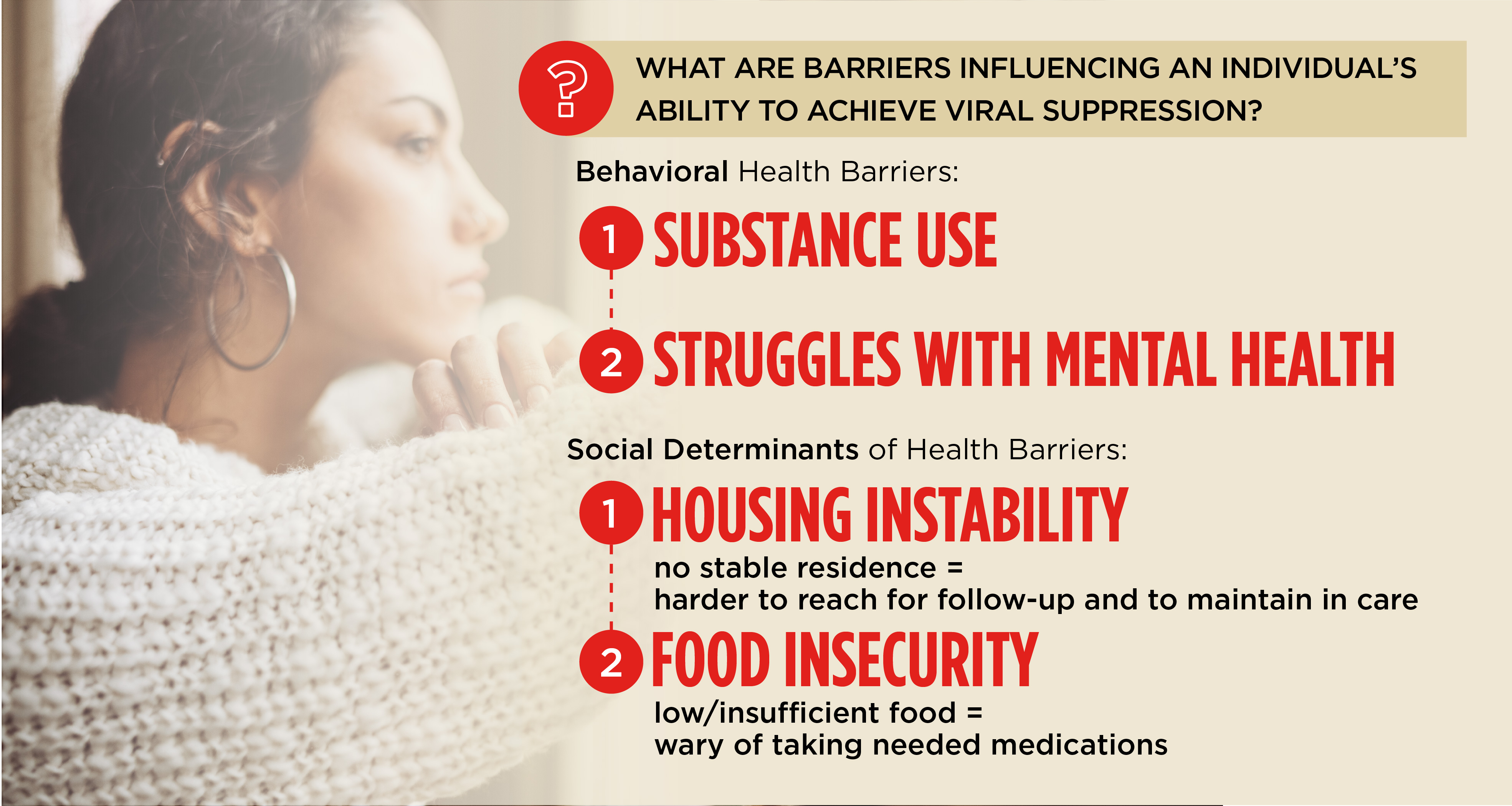
The Role of Social Determinants of Health on Achieving Viral Suppression
Despite improvements in testing, linkage, and retention, a significant number of Ryan White clients are not achieving viral suppression. That’s particularly true for young people and adults with unstable housing situations, living in poverty, and without health insurance. To understand the unmet needs of these vulnerable populations, Abt studied the interaction of viral resistance, co-morbidities, and social determinants of health. Drawing from a sample of 25 RWHAP provider sites, the Abt team conducted staff interviews, administered a validated trauma scale with clients, and facilitated client focus groups. We then analyzed the data with national RWHAP client demographics, service utilization, and HIV outcomes data, in combination with a survey of about 500 RWHAP providers.
Project Ryan White HIV/AIDS Program
Funder Health Resources and Services Administration (HRSA)
Understanding Barriers to Care Among High-Risk Populations
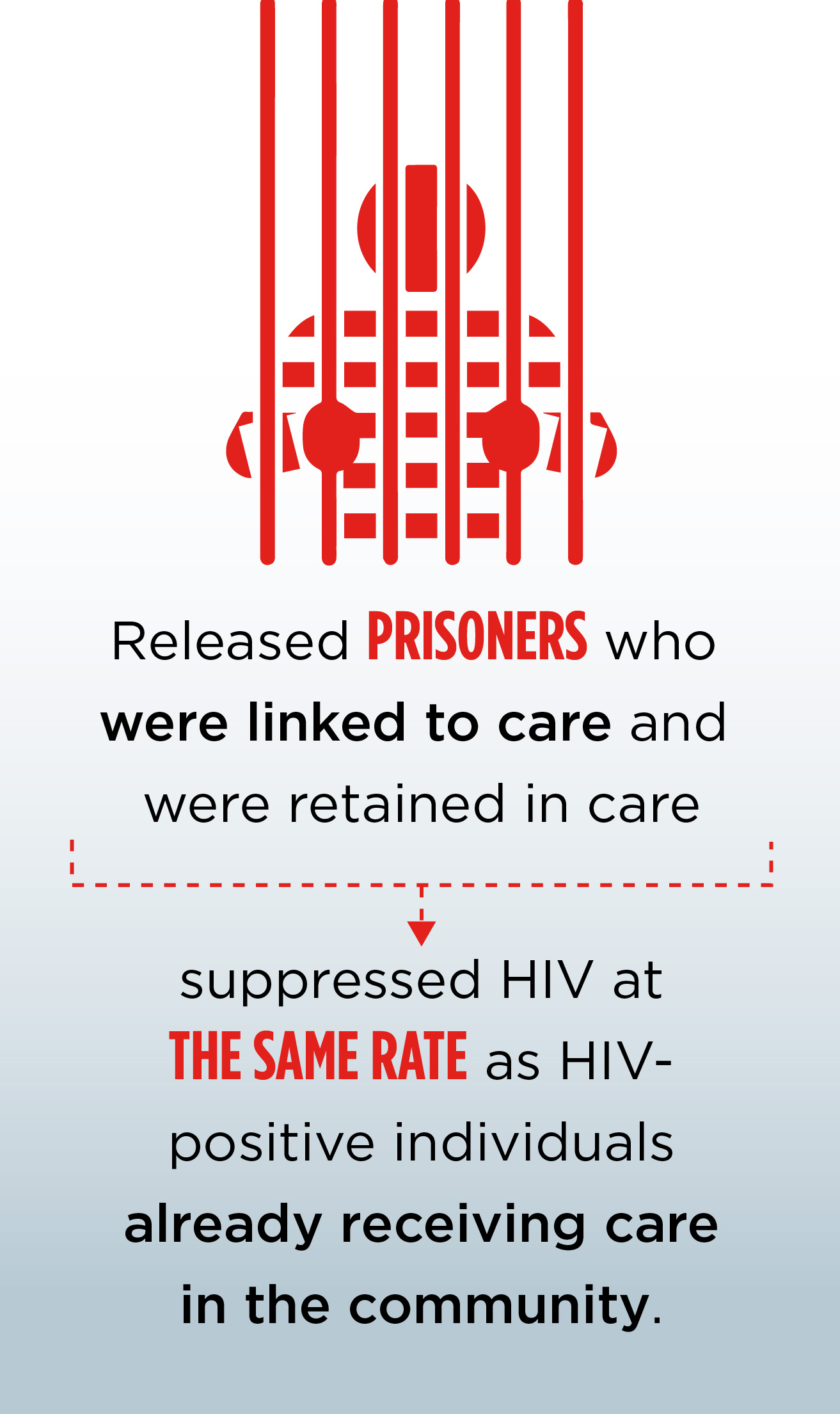
In the U.S., the prevalence of HIV among people in correctional facilities remains much higher than in the general population. Although the benefits of HIV treatment in jail are well understood, upon release, individuals often experience significant disruptions in HIV care. Abt evaluated the effectiveness of various methods of linking HIV+ persons post-release to primary medical care and ancillary services in their communities. A key finding from one of the studies showed that released prisoners who were linked to care and were retained continued to suppress HIV at roughly the same rate as HIV-positive individuals already receiving care in the community. The finding suggests that devoting resources to promoting such HIV care links and retention after release from prison would be money well spent.
Project Enhance Linkages to HIV Primary Care and Services in Jail Settings
Funder Miriam Hospital and the National Institute on Drug Abuse (NIDA)
Improving understanding of barriers for providing HIV care to high-risk populations—including MSM and transgendered women—is critical.
For the U.S. Substance Abuse and Mental Health Services Administration, Abt conducted two large outcome studies of the integration of primary care, mental health, and substance abuse treatment for at risk populations—the 11 Target Cities project and the evaluation of more than 175 grantees under the Minority AIDS Initiative-Targeted Capacity evaluation. Both of these large efforts highlighted the need for outreach to underserved populations and the vital need for an inclusive “no wrong door” approach to providing services. Engagement and retention on treatment services was especially low for women and transgender individuals.

Project HIV/AIDS Evaluation
Funder Substance Abuse and Mental Health Services Administration (SAMHSA)
MSM bear a disproportionate share of the HIV burden in the U.S.. Working with more than 20 partners throughout the country, Abt provided HIV testing and linkage services to reach more than 70,000 MSMs. We documented effective strategies and best practices in reaching men and assessing the cost effectiveness of different strategies. Building on this research, Abt evaluated the relative effectiveness of strategies for identifying previously undiagnosed HIV-positive African American MSMs.
We also explored strategies for motivating them to be tested for HIV and linked to medical care and prevention services. Abt developed and implemented two new outreach strategies to reach African American MSM. The first one was modeled on the structure of the social network projects funded through the Centers for Disease Control and Prevention’s Advancing HIV Prevention Initiative. The other, the Alternate Venue Testing, relies on providing HIV testing near where people live or socialize.
Project Scaling-up HIV testing Among African American and Hispanic MSM: The MSM Testing Initiative (MTI)
Funder Centers for Disease Control and Prevention (CDC)
Transgender women have a high risk for HIV infection and transmission, with an estimated prevalence rate of 28 percent. Yet little research has been conducted to understand the unique complexities surrounding transgender women’s experiences related to HIV prevention, care, and treatment. Abt partnered with Atlas Research to design a mixed-methods study with HIV-positive transgender women, HIV-negative transgender women, and healthcare providers in three U.S. cities. The goal was to ensure HIV prevention, treatment, and care strategies are effective and culturally appropriate.
Project Barriers and Facilitators to HIV Prevention, Care and Treatment Among Transgender Women
Funder Centers for Disease Control and Prevention (CDC)
