Tuberculosis


Tuberculosis (TB) is treatable and curable. Yet in 2018, the disease afflicted an estimated 10 million people around the world, deadlier than HIV/AIDS and malaria combined. Threats to effective TB control include poor detection, ineffective health system mobilization, and stigma. Increasing TB detection rates and then keeping people on treatment until they are cured are fundamental goals, and provide the best chance of staving off the growing threat of multidrug-resistant TB (MDR-TB).
Abt is putting people at the center of the solution. Facilitating systematic TB screening where people go to seek care first, destigmatizing the disease, eliminating barriers to treatment, and reducing diagnosis turnaround time—these are key strategies to measurably reduce the burden of TB across vulnerable communities.
Leveraging the Private Sector in Nigeria
Nigeria has one of the highest burdens of TB in the world, with 429,000 people contracting the disease in 2018 alone. As in many high-burden countries, TB testing and reporting are lengthy processes, primarily relying on paper records, overburdened labs, and slow data transit systems. This greatly impedes the country’s ability to account for and treat TB patients promptly. The government of Nigeria fights TB through its National Tuberculosis and Leprosy Control Programme (NTBLCP), which is primarily public sector-based. Strengthening the NTBLCP’s ability to detect TB is critical. With 70 percent of Nigerians seeking care in the private sector first, it is imperative that Nigeria’s private health sector be, integrated into the screening, diagnosis, and treatment of TB.
To harness the reach of the private sector, Abt facilitated a memorandum of understanding (MOU) between the government of Nigeria and private clinics, labs, pharmacies, and patent and proprietary medicine vendors in the two largest and highest TB-burdened states—Lagos and Kano. The MOU allows private health facilities to access the government’s TB drugs, kits, and GeneXpert-equipped labs to provide TB diagnosis, care, and treatment.
Building on the innovative network model Abt implemented in India through the Abt-led USAID Sustaining Health Outcomes through the Private Sector (SHOPS) project—which successfully leveraged the private sector in the fight against TB—Abt established a similar network model in Nigeria. Patent and proprietary medicine vendors, laboratories, pharmacists, and clinician-owned facilities are now connected through data sharing and logistics to ensure a continuum of care for TB patients. Direct South-to-South learning between India and Nigeria resulted in lessons shared and applied across countries to improve public-private mix models of TB care.
Working with the network providers, we’re building capacity to improve TB detection rates and boost the quality of referrals and treatment. We are streamlining follow-up through better collection and use of TB service delivery data, and real-time notifications. The results to date? In just one year—between October 2018 and September 2019—nearly 5,000 cases of TB were diagnosed through the private networks. More than 4,200 TB kits were distributed across the network providers, and 939 patients have already successfully completed their TB treatment.
Project Sustaining Health Outcomes through the Private Sector Plus (SHOPS Plus)
Funder U.S. Agency for International Development (USAID)
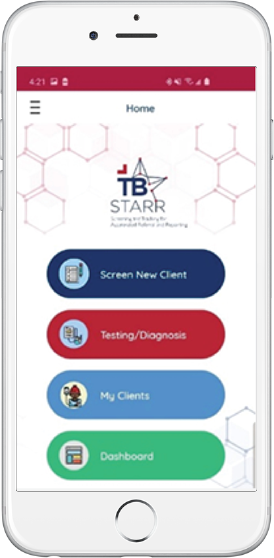
A digital solution to streamline the TB response
Accurate data and timely exchange of information can mean the difference between curing a case of TB and spreading the disease to dozens of additional community members. Countless paper registers scattered across independently run facilities obscure a clear view of a patient’s path towards timely detection and effective treatment. Zeroing in on this challenge, Abt launched TB STARR – an Android-based mobile app that enables real-time reporting and analysis of TB screening and diagnosis, all the way through treatment. The app also enhances notification to the national TB program of presumptive and confirmed TB patients, helping the national TB program secure an accurate supply of life-saving medicine. An additional non-networked provider version of the app enables the public-private partnership to be extended to clinical practitioners across 14 additional states, expanding NTBLCP’s reach and improving access to TB screening and treatment for millions of more Nigerians.
Project Sustaining Health Outcomes through the Private Sector Plus (SHOPS Plus)
Funder U.S. Agency for International Development (USAID)
Enabling a System-Wide, Sustainable Response to TB in Central Asia
Abt has been working to strengthen health systems in Central Asia and Eastern Europe since the 1990s. Through a series of USAID-funded projects, we contributed to significant improvements in health, including a dramatic decrease in TB mortality in Kazakhstan and Tajikistan of nearly 80 percent.
Project ZdravReform, ZdravPlus and ZdravPlus II
Funder U.S. Agency for International Development (USAID)
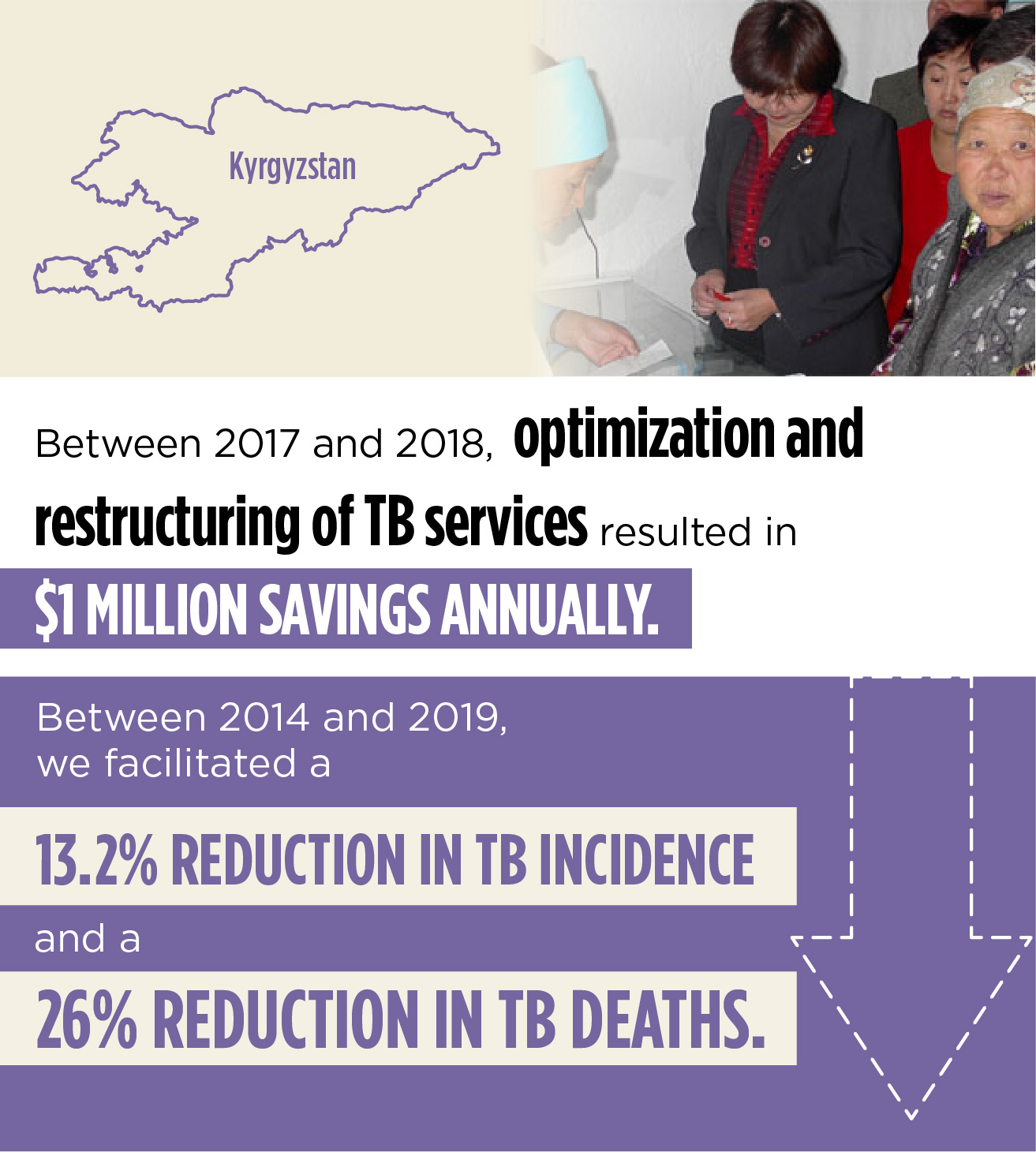
In the 2010s, Kyrgyzstan, a country of 6 million, was experiencing a dangerous rise of MDR-TB as a result of factors such as an inefficient hospitalization model, low-quality services, and lack of support to help TB-affected individuals access and stay on treatment until they are cured.
Abt applied a holistic health system strengthening approach to address Kyrgyzstan’s persistent TB challenges. We focused on strengthening community-level supports for the most vulnerable, eliminating harmful stigmas, streamlining logistics to reduce test-to-notification time, and facilitating the transition from expensive hospitalization to quality outpatient care. These interventions saved a million dollars annually, drove down the incidence of TB and decreased mortality by 26 percent.
To reduce test-to-notification time, we rolled out new transportation systems for TB samples, decreasing the average time between collection of sputum and notification from three weeks to two days. This got patients on treatment sooner and reduced the window for infected individuals to transmit the disease to others. For complex TB cases, we enabled expert TB committees to review cases via a new video teleconference system. Focusing on labs specifically, we established a quality management system that reduced the laboratory turnaround time from seven days to just three.
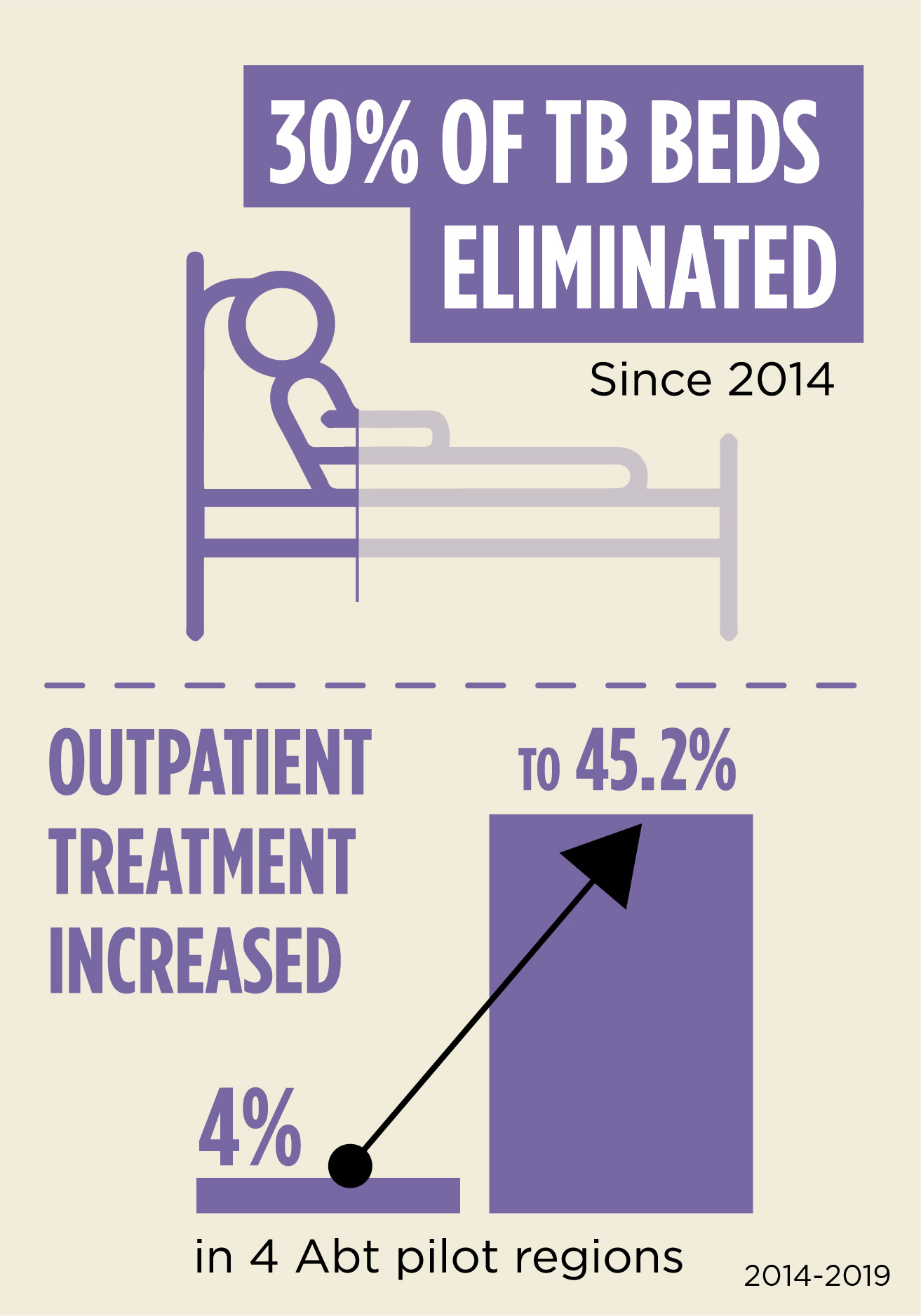
To transition Kyrgyzstan from expensive hospitalization to quality outpatient TB care, Abt worked closely with the government to evaluate the rate of unnecessary TB hospitalizations across the country, and shift those cases to outpatient centers. A case-based payment system that pays TB hospitals based on types of cases was also introduced. The system reduces the number of inappropriate admissions, encourages shorter lengths of stay and enhances the quality and safety of TB treatment. Since 2014, a total of 30 percent of TB beds have been eliminated and outpatient treatment increased from 4 percent to 45.2 percent in the four pilot regions Abt worked in.

To engage the whole community in the fight against TB, Abt built the structural and financial management capacity of civil society organizations so that they can more effectively advocate for and support the most vulnerable in their communities. To reduce stigma, address discrimination, and improve local understanding of TB, we engaged with local media, Village Health Committees, and community and religious leaders.
Increasing the rate of treatment adherence is critical to reducing the rise of drug resistant TB (DR-TB). We introduced and institutionalized the Community-based Treatment Supporter approach by mobilizing local volunteer community members and building their capacity to oversee patients’ daily TB treatment. Patients can take their drugs when and where it is convenient, and health workers can see their TB patients once a month instead of every day. This enables patients to complete their treatment more easily, increasing their TB regimen completion rate.
Project Defeat TB
Funder U.S. Agency for International Development (USAID)
Enabling Delivery of High-Quality TB Services in Papua New Guinea
Papua New Guinea (PNG) has the 10th highest TB incidence in the world. Nearly 30,000 people are diagnosed with TB annually, and the disease kills more people in PNG than any other infectious disease. Children account for a quarter of PNG’s TB cases, compared to 10 percent worldwide. In 2017, WHO classified PNG as one of only 14 countries that has a triple high burden of DR-TB, MDR-TB, and TB-HIV co-infection. Cases of extensively drug resistant TB (XDR-TB) also exist.
Working with the Australian government, Abt has been supporting the PNG government’s national strategy to address the TB epidemic through coordinated efforts with non-government organizations, including the private sector and community partners. Abt facilitates the provision of Australian government resources to the most affected areas, focusing on the elimination of DR-TB and the provision of treatment and preventative care to those most vulnerable. The strategy sets out ways to make TB services easier to access—including setting up TB health posts in high- burden communities and conducting health provider household visits—and to improve TB detection by installing new x-ray machines and improving laboratory facilities and equipment.
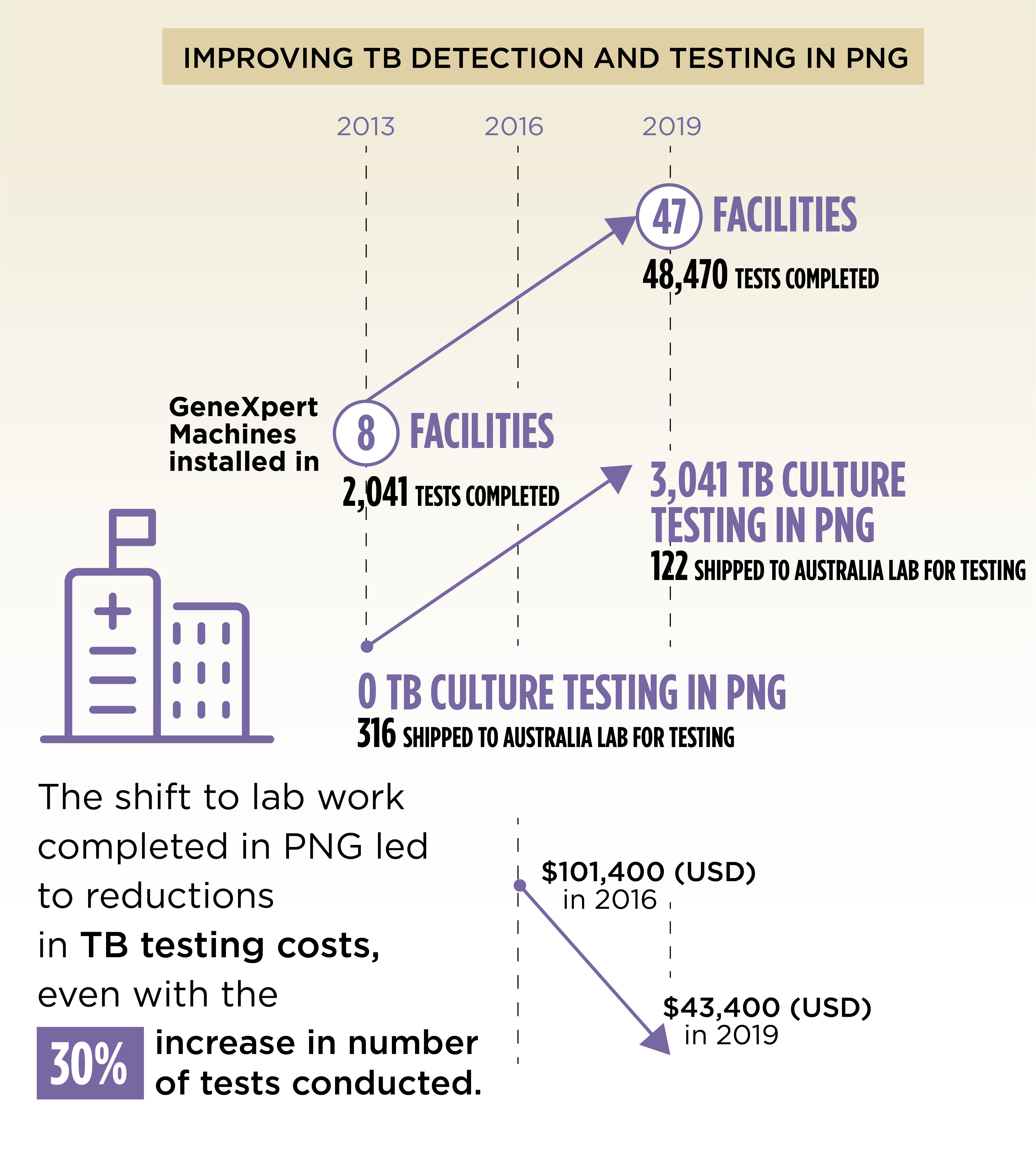
An independent review in late 2018 described Australian-funded initiatives as an excellent investment resulting in a substantial impact on the PNG TB burden. Strengthening the laboratories has resulted in reduced turnaround times for diagnosis and increased capacity for lab testing in PNG. The turnaround time from testing to treatment was reduced from 35 to 10 days at Port Moresby General Hospital and down to two days in Daru, Western Province.

Operational research has led to novel approaches to implementing effective screening, management of household contacts, and presumptive treatment regimens of new child-friendly medication. For example, an intensive household screening program in Daru had strong uptake, with 8-10 family members being screened for every active DS-TB and DR-TB case. All newly identified cases started treatment, and 70 percent of child contacts were placed on preventative therapy.
The establishment of directly observed therapy (DOT) strategies—in which community-based treatment sites are established to provide treatment support and food vouchers—eased the burden on hospitals and improved accessibility, especially for women and other vulnerable populations. These strategies resulted in a near gender parity for TB identification, while globally, low-income countries on average identify two male cases for every one female TB case.
Project Health and HIV Implementation Service Provider (HHISP)
Funder Australian Department of Foreign Affairs and Trade (DFAT)
